ABSTRACT
Objective: To evaluate the efficacy of verapamil in controlling hemodynamic responses to tracheal intubation under general anesthesia.
Methods:
We studied eighty normotensive patients (American Society of
Anesthesiologists physical status (I)) undergoing elective surgery. They
were randomly assigned to two main groups. Group I included 20 patients
randomly allocated into two equal subgroups (1a and 1b). Group II were
divided into three subgroups with 20 patients each (IIc, IId and IIe) to
receive saline (control), verapamil 0.05milligrams/kilogram body
weight, verapamil 0.1 milligrams /kilogram body weight. Patients with
anticipated difficult tracheal intubation, hypertension, renal or
hepatic diseases were excluded. The drugs were administered 60 seconds
before commencing laryngoscopy. Anesthesia was induced with thiopentone 5
milligrams/kilogram body weight intravenously and fentanyl 2mcµg/kg
intravenously, vecuronium 0.15 milligrams/kilogram body weight. During
anesthesia, ventilation was assisted or controlled with 1% halothane and
50% nitrous oxide in oxygen. Laryngoscopy lasting 30sec. was attempted 2
minutes after administration of thiopentone and vecuronium.
Results:
Patients receiving saline exhibited significant increase in systolic,
diastolic arterial pressures, mean arterial pressure, and heart rate
associated with tracheal intubation.
The increases in mean arterial
pressure and heart rate were attenuated in patients treated with
verapamil. These findings suggest that bolus injection of verapamil was
an effective method of controlling hypertension and tachycardia
associated with intubation.
Conclusion: This technique may
be useful in hypertensive patients and it may protect them from serious
complications. Further studies in hypertensive patients might be
helpful.
Key words: Cardiovascular responses, Laryngoscopy, Verapamil, Tracheal intubation.
JRMS June 2003; 10(1): 49-52
Introduction
Catecholamines exist in the circulation both as free catecholamines and as the sulphur conjugate that accounts for 60-90% of the total catecholamines (1). The serum levels of the catecholamines norepinephrine (2), epinephrine (3), and dopamine (2) have been observed to increase after a variety of stresses, including anxiety, hypotension, hypothermia (4), hypercarbia, and accidental injury. Plasma epinephrine concentrations reflect adrenomedullary secretion. Russell et al found that there are significant increases in arterial pressure and plasma norepinephrine concentration following intubation (5), so laryngoscopy and tracheal intubation provoke sympathetic response, which may result in tachycardia, hypertension and arrhythmias (6). Such cardiovascular disturbances although transient, may be dangerous in some patients, particularly those suffering from myocardial or cerebrovascular disease.
This stress response may be attenuated by uploads, or adrenergic blocking agents, ganglionic blocking and vasodilating agents including nitroglycerine, sodium nitroprusside, and calcium antagonists such as nifedipine, nicardipine and verapamil.
In this study the efficacy of verapamil in attenuating the cardiovascular responses to tracheal intubation was investigated.
Methods
We studied 80 patients meeting the physical status I of the American Society of Anesthesiologists (ASA) undergoing elective surgery. In 20 patients (group Ia, Ib) we studied the effects of single i.v. injection of verapamil on blood pressure (BP) and heart rate (HR) under anesthesia in the absence of stimulation produced by tracheal intubation.
Premedication was pethidine 50 mg and atropine 0.01mg/ kg i.m. 30 minutes before the induction of anesthesia that was induced with thiopentone 5mg/ kg, fentanyl 2 mcg /kg and vecuronium 0.15mg /kg then intubation was done 2 min later. Anesthesia was maintained with 1% halothane and 50% nitrous oxide in oxygen. Ventilation of the lungs was controlled to maintain end-tidal carbon dioxide partial pressure at 4.0- 5.1 KPa. After mean arterial pressure (MAP) and HR had stabilized, the patients were randomly allocated into two groups and given either 0.05mg/kg (group Ia) or 0.1mg/kg (group Ib) as a single i.v. injection. MAP was monitored via a radial artery cannulation, and HR and ECG were recorded. All measurements were completed before skin incision. Sixty normotensive (group II c, d, e) patients were randomly allocated into three groups of 20 patients each. Premedication was 50mg pethidine and atropine 0.01 mg/ kg i.m. 30 minutes before the induction of anesthesia. In the operating room, a radial arterial cannula was inserted under local anesthesia for continuous monitoring of MAP.
HR and ECG were monitored by lead II. After a 10minute stabilization period, the patients breathed 100% oxygen via a mask for 3 minutes. Immediately before induction of anesthesia, MAP and HR were recorded.
Anesthesia was induced with thiopentone 5mg /kg, fentanyl 2 mcg/ kg followed by 0.15 mg/kg to facilitate tracheal intubation. Direct laryngoscopy was attempted 2 minutes after induction, and tracheal intubation was completed within 30 sec in all patients. Verapamil 0.05 mg/ kg (group IId), 0.1mg /kg (group IIe) or Saline (group IIc) was injected 45 seconds before direct laryngoscopy. All tracheal intubations were performed by the same person. After induction of anesthesia, ventilation of the lungs was assisted or controlled with 1% halothane and 50% nitrous oxide in oxygen and end-tidal carbon dioxide partial pressure 4.1-5 KPa. MAP and HR were compared in the three groups (IIc, IId, IIe) and with pre-induction measurement.
Statistical analysis:
Data were analyzed by the analysis of variance (ANOVA) and P<0.05 was deemed significant.
Results
The five groups were comparable in age, weight and gender, as shown in Table 1.
In group I (a, b) MAP decreased significantly after verapamil in a dose-dependent manner 20 seconds after administration, reached its minimum after 90 sec. and return towards control was apparent by 4 minutes (Fig. 1) HR increased slightly but significantly, but there was no difference between the two doses. Hemodynamic variables are summarized in Table II.
In group II (c, d, e) there was no significant difference in MAP immediately before the start of laryngoscopy or before induction between the three groups (Fig. 2). In response to laryngoscopy and tracheal intubation, MAP increased significantly in all groups but the increase was significantly less in the verapamil treated groups than in the control groups. The larger dose of verapamil was associated with significantly greater attenuation of MAP than the smaller dose. (HR) increased in three groups after induction of anesthesia and immediately after tracheal intubation, and there was no significant difference between the three groups (Fig. 3). Verapamil at a dose of 0.1/mg kg had greater effect than 0.05-mg/kg. Hemodynamic variables are summarized in Table III. No patient was sufficiently hypotensive to require vasopressors.
The least MAP was 63.3 mm Hg (systolic 90-50). No abnormal ECG recording was observed in any patient.
Discussion
Perioperative cardiac complications are present and the incidence of postoperative myocardial ischemia can be reduced by using drugs (7).
We have found that verapamil 0.05mg /kg and 0.1mg /kg attenuated the increase in MAP; the inhibitory effect was greater with the larger dose. Hass and Hartfelder (8) showed that verapamil has a coronary vasodilator effect with negative inotropic and chronotropic effects. Verapamil dilates coronary, renal and hepatic arteries.
In common with other vasodilators, verapamil failed to prevent tachycardia caused by laryngoscopy and intubation, despite the negative chronotropic effect of the agent, which was masked by reflex sympathetic cardiac compensation induced by peripheral vasodilatation. The onset and duration of action of verapamil were rapid and transient, similar to the effects of other calcium channel blockers and vasodilators. Most drugs used to attenuate cardiovascular responses to intubation, including narcotics, calcium channel blockers, and beta-blockers, have been associated with hypotension (9). No patients in the current study had severe hypotension with any of the two doses. In a few patients in group Iia&IIb MAP reached 55 mm Hg which is hazardous even in ASA I patients. Some papers reported that a bolus dose of verapamil produced a dose-dependent reduction in MAP in ASA I patients undergoing general anesthesia (10). In clinical use, because laryngoscopy for tracheal intubation begins before verapamil has attained its maximal hypotensive effect, undue hypotension during induction of anesthesia can probably be avoided even when using a dose of 0.1mg/kg. A single i.v. administration of verapamil 5-10mg has been shown to decrease arterial pressure in hypertensive patients at rest and during exercise (11,12).
The magnitude of arterial pressure decrease caused by a given dose of verapamil is greater in hypertensive patients than in normotensive subjects (11,12).
Conclusion
This technique may be useful in hypertensive patients and it may protect them from serious complications and further studies in hypertensive patients might be helpful.
Table I: Demographic data of the study groups.
|
|
Ia
|
Ib
|
IIc
|
IId
|
IIe
|
|
Number
|
10
|
10
|
20
|
20
|
20
|
|
Sex (Male: Female)
|
6:4
|
5:5
|
11:9
|
10:10
|
8:12
|
|
Age range (year)
|
25-50
|
26-55
|
28-52
|
27-50
|
29-53
|
|
Weigh range (ilokgram)
|
50-75
|
48-70
|
42-65
|
45-73
|
94-69
|
Table II: Comparison of the relation between MAP and HR with time after administration of verapamil in group I.
|
*Time (min)
|
0
|
1
|
2
|
3
|
4
|
5
|
|
**MAP
|
|
I a mmHg
|
98-110
|
90-103
|
78-83
|
83-90
|
90-104
|
104-108
|
|
I b mmHg
|
100-106
|
83-105
|
68-75
|
70-91
|
88-98
|
97-105
|
|
^HR
|
|
I a beats/min.
|
74-85
|
81-90
|
92-105
|
89-101
|
80-93
|
70-78
|
|
I b beats/min.
|
68-80
|
29-103
|
95-115
|
89-98
|
75-89
|
65-77
|
* Time after administration of verapamil (min) ** MAP: Mean arterial pressure ^HR: Heart rate
Table III: Comparison of the relation between the MAP and HR with time after administration of verapamil after intubation in group II
|
Time (min)
|
0
|
1
|
2
|
3
|
4
|
5
|
|
**MAP
|
|
II c mmHg
|
80-97
|
74-95
|
72-97
|
113-131
|
90-108
|
90-108
|
|
II d mmHg
|
84-99
|
78-87
|
72-84
|
98-122
|
93-110
|
87-100
|
|
II e mmHg
|
86-101
|
80-90
|
69-82
|
92-119
|
88-108
|
86-102
|
|
^HR
|
|
II c beats/min
|
69-87
|
76-95
|
79-98
|
101-109
|
88-103
|
80-101
|
|
II d beats/min
|
71-80
|
74-91
|
81-89
|
84-116
|
82-98
|
77-85
|
|
II e beats/min
|
65-77
|
71-88
|
78-95
|
92-109
|
76-104
|
71-92
|
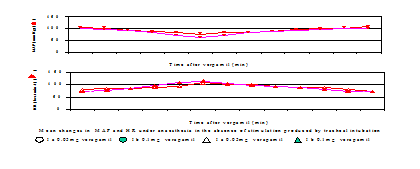 Fig. 1:
Fig. 1: Relation between MAP and HR after verapamil at different times.
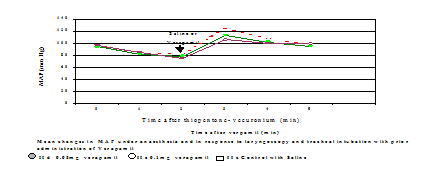 Fig. 2:
Fig. 2: Relation between MAP after verapamil and saline (control) after intubation at different times.
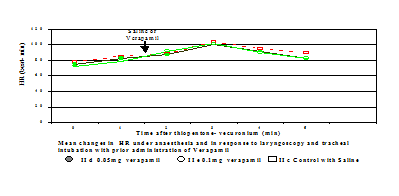 Fig. 3:
Fig. 3: Relation between HR after verapamil and saline (control) after intubation at different times.
References1.
Woolf PD, Hamill RW, Lee LA, McDonald JV. Free and total catecholamines in critical illness. Am J Physiol 1988; 254: 287-291.
2.
Davies CL, Malyneuf SG, Newman RJ. HPLC determination of plasma catecholamines in road accident casualties. Br J Clin Pharmacol 1981; 13: 283.
3.
Frayn KN, Little RA, Maycock PF, Stoner HB. The relationship of plasma catecholamines to acute metabolic and hormonal responses to injury in man. Circ Shock 1985; 16: 229-240.
4.
Benedict CR, Graham-Smith DG. Plasma noradrenaline and adrenaline concentrations and dopamine beta hydroxylase activity in patients with shock due to septicemia, trauma, and hemorrhage. J Med 1978; 185: 1-20.
5.
Russel WJ, Morris RG, Frewin DB, Drew SE. Changes in plasma catecholamine concentrations during endotracheal intubation. Br. J Anaesthesia 1981; 53: 837-839.
6.
Ng WS. Pathophysiological effects of tracheal intubation
In: Latto IP, Rosen M, Eds. Difficulties in Tracheal Intubation. Eastbourne: Bailliere Tindall, 1985; 12-35.
7.
Wallace A, Layug B, Ida Tateo I, et al. Prophylactic atenolol reduces postoperative myocardial ischemia. Anesthesiology 1998; 88: 7-17.
8.
Hass H, Hartfelder G. Alfa-isopropyl-alfa. A Rzneimittel Forschung 1962; 12: 549-558.
9.
Yoo KY, Lee J, Kim HS, Woong M. Hemodynamic and catecholamines responses to laryngoscopy and tracheal intubation in patients with complete spinal cord injuries. Anesthesiology 2001; 95: 647-651.
10.
Khan RM, Khan TZ, Hakim S, et al. Verapamil as a hypotensive agent under general anesthesia, Journal of The Indian Medical Association 1990; 88: 251-253.
11.
McTavish D, Sorkin EM. Verapamil an updated review of its pharmacodynamic and pharmacokinetic properties, and therapeutic use in hypotension. Drugs 1989; 38: 19-76.
12.
Frishman WH, Weinberg P, Peled HB, et al. Calcium entry blockers for the treatment of severe hypertension and hypertensive crisis. Am J Med 1984; 35-45.