Objective: To evaluate the diagnostic
accuracy of scintimammography using 99m Technetium -
methoxyisobutylisonitrile (99mTc-MIBI) in the detection of breast cancer
in comparison with conventional mammography.
Methods: A
total of 113 patients with clinically suspicious breast masses and/or
positive mammograms suggesting breast cancers were included in this
study. After 10 minutes of 99mTc-MIBI injections, one anterior image in
the prone position and two lateral prone images were acquired for 10
minutes each. Another set of images was taken in the same position
after 60 min of injection.
Results: One-hundred and
nineteen lesions (92 palpable and 27 non-palpable) were detected. There
were 75 malignant and 44 benign lesions according to the histopathology
findings obtained during excisional biopsies. The relation with the
histopathology showed that the overall sensitivity and specificity of
scintimammography were 68% and 73% respectively. However for palpable
lesions, the sensitivity and specificity were 79% and 76%,
respectively. Sensitivity was not dependent on the density of the
breast tissue.
The sensitivity and specificity of mammography were 89% and 43% respectively, and did not depend on the tumor size.
In 60% of false-negative mammograms, 99mTc-MIBI was able to diagnose malignancy (True-positive).
Conclusion:
Imaging with 99mTc-MIBI showed a high diagnostic accuracy for the
detection of breast cancer and could be used as a complementary imaging
modality to conventional mammography in diagnosing breast cancer at an
earlier stage particularly in patients with dense breasts.
Key words: Scintimammography, 99m Technetium –methoxyisobutylisonitrile,
JRMS Dec 2003; 10(2): 18-23
Introduction
Breast cancer is the commonest cancer in women. It accounts for the highest proportion of cancer-related deaths (1). There has been a rise in the incidence of this malignant disease over recent years (2); especially in younger age groups. Early detection and diagnosis are crucial allowing for treatment in early stages, and improving survival times by reducing the associated morbidity and mortality (3).
Mammography is the commonly used technique for early detection of breast cancer. Its main limitation is represented by its low positive predictive value with many biopsies revealing benign lesions (4). It has a lower detection rate in women with large or highly fibroglandular breasts or with retroglandular lesions or where breast implants are present (5).
Recently, encouraging results have been obtained by means of nuclear breast imaging using different radiopharmaceuticals such as 99m-technetium methoxyisobutylisonitrile (99mTc-MIBI), fluorine-18 fluordeoxyglucose, thallium-201 chloride, Tc-99m-Methyl Diphosphenate (MDP) and others (6-12), 99mTc-MIBI, a cardiac perfusion agent used in the detection of coronary artery diseases (13), has been shown to be of great value in the detection of various malignancies (14-17). More recent studies have demonstrated a high diagnostic accuracy of 99mTc-MIBI in the detection of breast cancer (18-23). This study was conducted to confirm the diagnostic value of scintimammography using 99mTc-MIBI in breast cancer detection.
MethodsPatientsOne hundred and thirteen female patients aged (27-63) with a mean age of 51 years were studied. Of these, 78 patients had breast abnormalities detected by physical examination. The remaining 35 patients had non-palpable breast abnormalities detected by mammography performed because they belonged to high-risk groups or as part of routine oncological follow-up.
All the patients included in this study were older than 25 years, not pregnant, non-lactating and also signed an informed consent prior to their examination. Sixty three percent of patients were postmenopausal. Mastectomy and lumpectomy of the contralateral breast was carried out in 2% and 1% of patients respectively. Excisional or fine needle biopsy had been performed in all patients. Patients with either previous mastectomy of the breast with suspicious lesion, local tumor recurrence or with fine-needle biopsy within one-week prior to scintimammography were excluded from the study.
The total number of lesions was 119, 82 were detected by palpation and the remaining 37 were detected by mammography. The overall ratio of palpable to mammographically detected lesions was approximately 2.2:1.
Only six patients had two pathological lesions of the breast.
ScintimammographyScintimammography was performed using a commercial agent, Cardiolite. 99mTc-MIBI is supplied in 5 ml vials containing lypholized material and its preparation requires reconstitution with 99mTc-pertechnetate followed by heating in a water bath. The radiochemical purity of the kit should be greater than 90%.
Each patient received an intravenous injection into the arm on the side contralateral to the breast lesion. The average dose was 20 mCi (range 18 - 30 mCi).
Planner imaging was started 10 min after the injection of 99mTc-MIBI. The imaging sequence was as follows: First, 10 min anterior view with the patient in the prone position while her arms raised behind her head (Fig. 1, 2). Second, 10-min lateral view to the breast with the suspected lesion while the patient is lying on her side. Third, 10-min lateral view to the other breast following repositioning of the patient (Fig. 3, 4). Finally, delayed imaging 1-hour post injection (24).
Planner images were performed with 256X256 image matrix, a 10% window and an energy peak of 140 KeV. A low-energy high-resolution collimated gamma camera without zoom was used. The camera was positioned as close as possible to the breast. A maximum of four images were assessed for each lesion; an initial and a delayed image for both lateral and anterior prone views (22). One reader assessed each set of images as follows: Normal if there was no uptake, equivocal, or positive if there was an uptake regardless of its intensity. Regarding the primary assessment of diagnostic accuracy, any breast with positive uptake was interpreted as a positive result (definition 1). A secondary assessment was also made in which a positive result was assumed if there was either equivocal or positive uptake (definition 2).
Fig. 1: 99m-TC-MIBI anterior image of the breast showing a focus of increased uptake in the right breast.
 Fig 2:
Fig 2: Anterior image with Tc-99m-MIBI showing a large fungating and highly malignant breast mass.
 Fig. 3:
Fig. 3: Lateral view with a pinhole collimator showing an abnormal focus of Tc-99m-MIBI uptake in the left breast.
 Fig 4:
Fig 4: Lateral view showing an abnormal focus of Tc-99m-MIBI uptake in an axillary lymph node.
MammographyAll patients were initially studied using mammography where craniocaudal (Fig. 5) and mediolateral oblique views were performed for each breast using Siemens Mammomat 2 machine. Patients were classified according to their mammographic findings into negative, suspicious, and positive for malignancy. The suspicious group was considered to be the true positive for predicting malignancy since these patients underwent histopathological examinations.
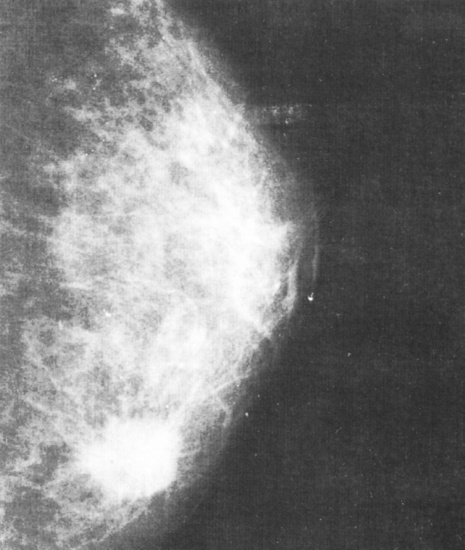 Fig 5:
Fig 5: Craniocaudal view of the Lt. breast showing a stellate mass in the inner quadrant of the (breast carcinoma)
HistopathologyHistopathological and cytological confirmation was obtained by means of excisional biopsy in 67 patients and fine needle aspiration in 46 patients within 3 weeks following scintimammography study. Lesions were classified either as benign or malignant. All patients with inconclusive histopathological results were excluded from this study.
Data analysisThe patients in this study had to meet the following criteria to be included in the efficacy population:
- Had a standard mammographic examination.
- Received the 99mTc-MIBI imaging agent.
- Had a biopsy for which a microscopic diagnosis existed.
All efficacy analyses were made separately for each target group of patients regarding breast abnormalities detected either by palpation or mammography.
The measurement of agreement between any two of the assessment methods was based on a (2X2) table in which one of the classifying factors was the gold standard (e.g. histopathological results). The following statistics were derived from these tables including sensitivity, specificity, overall agreement, positive predictive value (PPV) and negative predictive value (NPV).
An advanced assessment used to indicate whether one technique is better than the other was based on a (4X4) table and included false negative, false positive, true negative and true positive results of the methods.
Several different types of assessment were used to evaluate the diagnostic accuracy of sestamibi imaging with that of mammography, to establish whether the diagnostic performance of the imaging technique can be improved by modifying the method of interpretation and to ascertain whether the use of the two techniques, scintimammography and mammography, in conjunction provides a better predictive capability than either technique used alone.
Results
Histopathological findingsBased on the final histopathological diagnosis, 75 lesions were diagnosed as malignant and 44 as benign. There were 58/75 palpable malignant lesions and 34/44 palpable benign lesions (Table I).
Scintimammographic resultsWhen these results were compared with the histopathological results (Table I), scintimammography was true-positive in 51 out of 75 cancers. This resulted in an overall sensitivity of 68% (Table I). In this group, sensitivity for palpable and non-palpable cancers was 79% and 29% respectively. The overall specificity was 73% (12/44 false positive scans). The specificity was 76% for palpable lesions and 60% for non-palpable lesion. The positive predictive value and negative predictive value were 81% and 57%, respectively.
Mammographic resultsMammographic results were compared with histopathological findings (Table II), where mammography was true positive in 67 out of 75 cancers and true negative in 19 out of 44 benign lesions of the breast. This resulted in a sensitivity and specificity of 89% and 43% respectively (Table II). The sensitivity and specificity for mammography were 91% and 32% respectively for palpable lesions while it was 82% and 80% for non-palpable lesion respectivly. Both sensitivities and specificities for mammographic results are shown in (Table II). The PPV and NPV for Mammography were 81 and 575 respectively. Finally, if mammography and scintimammography results were compared (Table III), two cancers scored true positive by the scintimammography had been indicated as false negative by mammography. This means that in 25% of false negative scintimammography could diagnose the cancer.
Density of breastsSensitivity of scintimammography was independent of the density of breast tissue. Out of 75 cancers; 42 (56%) were categorized as located in a breast of mammographic grade I (fatty breast), 15 (20%) were located in grade II density and 18 (24%) were located in grade III density breast. The overall sensitivities of scintimammography for these groups were 71%, 73%, and 72% respectively, while the overall sensitivities for mammography were 95%, 93% and 75% respectively (Table IV).
Discussion
Recently, nuclear breast imaging has gained significant interest as several nucleotides have demonstrated promising results in the diagnosis of breast cancer. 99mTc-MIBI is a cationic complex, which can accumulate in the tumor cells (25). The accumulation of 99mTc-MIBI in the tumor is dependent on the quantity of mitochondria in the tumor cell, the electric membrane potential and the expression of the multidrug resistance (MDR) gene (26). Recent studies using 99mTc-MIBI for breast cancer detection have shown high sensitivity and specificity for palpable cancers (16,22,23). The diagnostic accuracy has been less favorable for non-palpable breast lesions (22,23). In this study, scintimammography using 99mTc-MIBI has achieved an overall sensitivity of 68%.
There are still significant limitations to the use of mammography for the detection of breast cancer; these limitations persist in spite of technical improvements facilitating diagnosis. Its diagnostic benefit is less favorable especially in younger women (less than 50 years old) with dense breasts (4,5). Thus there is a need for a non-invasive method to complement mammography and to differentiate between benign and malignant breast lesions in dense breast. Such a method should be reliable, with high sensitivity and high predictive value.
In this study, mammographic results were within the range of values reported in the literature (18,19). The overall sensitivity and specificity were 89% and 43% respectively. Sensitivity of mammography was observed to be slightly less in patients with non-palpable cancers. The overall sensitivity of mammography was scintimammography indicating that scintigraphy, in its current state, is not suitable for breast cancer screening.
However this study has shown that scintimammography could provide supplementary information to mammography and helped to detect breast cancer earlier in a subgroup of patients. In 25% of patients with false-negative mammogram, scintimammography could diagnose the breast cancer. This group was consisted of younger patients with mammographically dense breast tissue resulting in false negative mammogram.
This study was also able to prove that the diagnostic accuracy of scintimammography is independent of the density of breast tissue as reported by Khalkhali et al (22). Consequently premenopausal patients whose mortality from breast cancer cannot be decreased significantly by screening mammography will benefit most from scintimammography.
In the majority of cases, the woman herself detects any changes of the breast for which she consults her physician (28). Sensitivity of breast palpation is not satisfactory and often-lumpy breasts would make it difficult to characterize sufficiently a palpable nodule or mass in the breast (28). If mammography performed in further diagnostic work-up is indeterminate and a suspicion of malignancy is low, the patient will be advised to return for a control mammography in 3-6 months. In this group of patients, the majority of them are premenopausal women; scintimammography could help in diagnosing breast cancer at an earlier stage when it is used as a complementary method to mammography.
The exact localization of MIBI positive area remains a problem since neither planar imaging nor Single Photon Emission Computerized Tomography (SPECT) provides the surgeon with sufficient information for biopsy of breast tissue. When all other imaging modalities such as mammography, ultrasonography and magnetic resonance imaging are negative, scintimammography must be used for tumor localization. Khalkhali et al showed that the prone position with the breasts hanging freely is the best technique for the performance of lateral scintimammography because deeper regions of the breast can be visualized (22).
Regardless of which technique is used, the breast must not be compressed from either side. Furthermore, a high-resolution gamma camera should be used with acquisition time of more than 10 min if good quality images are to be obtained. Special attention must also be drawn to the distance between the collimator and the breast, which ideally should touch the camera surface. Standardization of scintimammography will help to achieve quality level of this technique.
Conclusion
Our results were in line with those previously reported in literature and they demonstrated a high diagnostic accuracy of 99mTc-MIBI scintimammography in the evaluation of palpable breast lesions. Sensitivity is independent of mammographically determined density of the breast tissue. Scintimammography is suitable as a complementary method to mammography in patients with dense breasts and also with intermediate or low probability of breast cancer. Finally, patients with a high risk of breast cancer may benefit from radionucleotide with 99mTc-MIBI.
Table I: Histopathology and Mammoscintigraphic results with their sensitivity and specificity.
|
Histopathology
|
Number of Lesions
|
Mammoscintigraphy
|
Sensitivity
|
Specificity
|
|
Positive
|
Negative
|
|
Malignant
|
Total
|
75
|
51
(TP)
|
24
(FN)
|
68%
|
73%
|
|
P
|
58
|
46
(TP)
|
12
(FN)
|
79%
|
76%
|
|
N-P
|
17
|
5
(TP)
|
12
(FN)
|
29%
|
60%
|
|
Benign
|
Total
|
44
|
12
(FP)
|
32
(TN)
|
|
|
|
P
|
34
|
8 (FP)
|
26
(TN)
|
|
|
|
N-P
|
10
|
4
(FP)
|
6
(TN)
|
|
|
Where P, N-P, TP, FN, TN, FP denotes palpable, non-palpable, true positive, false negative, true negative and false positive respectively.
Table II: Mammography results compared with histopathology and their sensitivity and specificity.
|
Histopathology
|
Number
of Lesion
|
Mammography
|
Sensitivity
|
Specificity
|
|
Positive
|
Negative
|
|
Malignant
|
Total
|
75
|
67 (TP)
|
8 (FN)
|
89%
|
43%
|
|
P
|
58
|
55 (TP)
|
3 (FN)
|
95%
|
32%
|
|
N-P
|
17
|
14 (TP)
|
3 (FN)
|
82%
|
80%
|
|
Benign
|
Total
|
44
|
25 (FP)
|
19 (TN)
|
|
|
|
P
|
34
|
23 (FP)
|
11 (TN)
|
|
|
|
N-P
|
10
|
2 (FP)
|
8 (TN)
|
|
|
P, N-P, TP, FN, TN, FP denotes palpable. Non-palpable, true positive, false negative, true negative and false positive respectively.
Table III: A comparison between mammographic and mammoscintigraphic results.
|
Mammographic
|
Scintigraphic
|
|
Results
|
|
TP
|
FP
|
FN
|
TN
|
|
TP
|
67
|
49
|
-
|
18
|
-
|
|
FP
|
25
|
-
|
6
|
-
|
19
|
|
FN
|
8
|
2
|
-
|
6
|
-
|
|
TN
|
19
|
-
|
6
|
-
|
13
|
Table IV: According to breast density; a comparison for the sensitivity for malignant lesions between mammography and mammoscintigraphy
|
Density
|
|
Number of cases
|
Sensitivity
|
|
MIBI
|
Mammography
|
|
I
|
Malignant
Benign
|
42
25
|
30(71%)
|
40(95%)
|
|
II
|
Malignant
Benign
|
15
7
|
11(73%)
|
14(93%)
|
|
III
|
Malignant
Benign
|
18
12
|
13(72%)
|
14(75%)
|
References
1. Berg JW, Hutter RV. Breast Cancer. Cancer 1995; 75: 257-269.
2. Byrne C, Smart C, Chu K, Hartman W. Survival advant age differences by age. Cancer Suppl 1994; 74: 301-310.
3. Kerlikowske K, Grady D, Barclay J. Likelihood ratios for modern screening mammography. Risk of breast cancer based on age and mammography interpretation. JAMA 1996; 276: 39-43.
4. Lannin DR, Harris RP. Difficulties in diagnosis of carcinoma of the breast in patients less than fifty years of age. Surg Gyneco Obstet 1993; 177: 457-476.
5. Covney EC, Geraghty JG. Reasons underlying negative mammography in patients with palpable breast cancer. Clin Radiol 1994; 49: 123-125.
6.
Burak Z, Argon M, Memis A. Evaluation of palpable breast masses with Tc-99m-MIBI: A comparative study with mammography and Ultrasonography. Nucl Med Comm 1994; 15: 604-612.
7. Uriarte I, Carril JM, Remedios Q, et al. Optimization of X-ray mammography and Tc-99m-methoxyisobutylisonitril scintimammography in the diagnosis of non-palpable breast lesions. Eur J Nucl Med 1998; 25: 491-496.
8.
AL-Nahhas AM, Mccready VR. The role of radionuclide studies in breast cancer. Nucl Med Comm 1993; 14: 192-196.
9.
Van Eijck CHJ, Kernning EP. [Editorial] Nuclear medicine imaging of breast cancer. Nucl Med Comm 1996; 17: 925-927.
10.
Adalet, MO, Demirkol M. Muslumanoglu. Tc-99m-tetrofosmin scintigraphy in the evaluation of palpable breast masses. Nucl Med Comm 1997; 18: 118-121.
11.
Chiti A, Agresil R. Breast cancer staging Tc-99m-sestamibi and In-111 pentetreotide single-photon emission tomography. Eur J Nucl Med 1997; 24: 192-196.
12.
Buscombe JR, Cwikla JB. Prone SPET Scintigraphy. Nucl Med Comm 1999; 20: 237-245.
13.
Chung G, Lahiri A. Myocardial perfusion imaging in modern cardiology. British Journal of Cardiology 2000; 7(10):619-623.
14.
Balon HR, Fink-Bennet DM. Technetium 99m-MIBI uptake by recurrent Hurtle cell carcinoma of the thyroid. J Nucl Med 1992; 33: 1393-1395.
15.
Moka D, Dietlein M, Voth E. Preoperative localization of parathyroid adenomas using Tc-99m-MIBI scintigraphy. American Journal of Medicine 2000; 108: 733-738
.
16.
De Jong CM, Bernard BF, Breeman W. Comparison of uptake of Tc-99m-MIBI, Tc-99m-Teterofosmin and Tc-99m-Q12 into human breast cancer cell lines. Eur J Nucl Med 1996; 23: 1361-1366.
17.
Koukourakei S, Damilakis J. Functional imaging of tumors with Tc-99m-sestamibi pinhole scintigraphy. Nucl Med Comm, 1996; 17: 943-951.
18.
Arslan N, Ozturk E, Ilgan S, et al. Tc-99m-scintimammography in the evaluation of breast lesions and axillary involvement: A comparison with mammography and histopathological diagnosis. Nucl Med Comm, 1999; 20: 317-325.
19.
Palmodo H, Biersack HJ, Lastoria S, et al. Scintimammography with Tc-99m-MIBI: Results of a prospective European multicenter trial. Eur J Nucl Med 1998; 25: 375-385.
20.
Parts E, Asia F, Abos MD. Mammography and 99mTc-MIBI in Suspected breast cancers. J Nucl Med 1999; 40(2): 296-301.
21. Horne T, Pappo I, Cohenpour M, et al. Tc-99m-MIBI scintimammography for the detection of breast malignancies: The contribution of the count ratio to specificity. Nucl Med Ccomm 1999; 20: 511-516.
22.
Khalkhali I, Cutrone JA. Scintimammography: The complementary role of Tc-99m sestamibi prone breast imaging for the diagnosis of breast cancer. Radiology 1995; 196: 421-426.
23.
Villanueva-Meyer J, Leonhard MH. Mammoscintigraphy with Tc-99m sestamibi in suspected breast cancer. J Nucl Med 1996; 37: 926-930.
24.
Lu G, Shih WJ, HY Huang. Tc-99m-MIBI Mammoscintigraphy of breast masses: Early and delayed imaging. Nul Med Comm 1995; 16; 150-156.
25.
Reilly RM, So M, Polihronis J. Rapid quality control of Tc-99m-sestamibi. 1992; 13: 644-666.
26.
Vecchio SD, Ciarmiello A, Potena MI. In Vivo detection of multidrug-resistant (MDR1) phenotype by Tc-99m-sestamibi scan in untreated breast cancer patients. Eur J Nucl Med 1997; 24: 150-159.
27.
Sciuto T. Tc-99m-MIBI scintimammography in 300 consecutive patients: Factors that may affect accuracy. Nucl Med Commun 1999; 20(12): 1113-1121.
28.
Donnegan WL. Evaluation of palpable breast mass. N Engl J Med 1992; 327