A five-year-old female with eight months history of fever diagnosed to have disseminated tuberculosis. Although she denied any respiratory or eye complaints, there were wide spread miliary infiltrates in the lungs and disseminated choroidal tubercles in the fundi.
JRMS Dec 2005; 12(2): 45-47
IntroductionDisseminated tuberculosis continues to be a challenge to physicians. It represents unchecked hematogenous dissemination of mycobacterium tuberculosis. It represents less than 2% of all TB cases (1). The manifestations are protean and may continue for months with little or slow progression (2). Herein we present clinical characteristics of disseminated TB in a 5-year-old girl.
Case Report
BA, a 5-year-old girl was admitted on the 19th of November 2000 with 8 months history of fever and night sweats and weight loss of 2 kg. The fever was remittent, associated with chills. She denied any history of cough and dyspnea and there were no gastrointestinal symptoms. Review of other systems was normal. She received five shots of DTP and Oral Polio vaccines and three Hepatitis B vaccines. She had neither HemophilusiInfluenza type B nor BCG vaccines. There was no history of contact with patients with open tuberculosis and other contagious diseases. There was no history of recent measles, Varicellaa and Pertussis. She was not a school attendant.
Four weeks prior to admission she had burning micturition and diagnosed to have Klebsiella spp. urinary tract infections and received one-week course of Septrin. The burning upon micturition disappeared but the fever persisted. At that time her hematocrit, WBC were normal and abdominal Ultrasound, and chest X-ray (CXR) reported normal. Her parents and four siblings were healthy.
Clinical examination revealed a cooperative girl with some pallor and temperature of 37o C orally. Her weight was 16 kg. Respiratory and heart rates were 20 breaths and 100 beat/min, respectively. Meningeal signs were negative. There was neither lymph nodes enlargement nor skin rashes. Chest examination was completely normal with good air entry bilateral and no crackles or wheeze. The heart was normal. The abdomen was soft lax and the liver was grossly enlarged with smooth surface and sharp edge 10 cm below costal margin. The spleen was just felt, genitalia and extremities were normal with no finger clubbing.
Chest X-ray showed diffuse miliary shadowing bilateral as shown in (Fig. 1). Peripheral blood counts and film were normal; ESR first hour was 13, 15, and 10 on three occasions. Liver and kidney functions were normal apart from some liver enzymes leak (AST and ALT were 110 and 120U, respectively).
C-reactive protein was 24. Brucella titer and rheumatological screen were negative. Viral serology for hepatitis A, B, C, EBV, and HIV viruses were negative. Cold agglutinin was 1/256. The Z-Nelson stains on three fasting gastric aspirates, taken on three consecutive days were negative for Mycobacterium tuberculosis. Five TU tuberculin test was negative. Two blood cultures were also negative. CSF analysis (cells, protein & sugar) and culture was negative for bacterial meningitis. Abdominal ultrasound showed gross hepatomegaly, mild splenomegaly, normal kidneys and some pelvic ascites, but no para-aortic lymph nodes enlargement. The pelvic ascites was not accessible for aspiration. She was given erythromycin 40-mg/ kg/day.
During the first week of hospitalization she showed remittent fever with 2-4 spikes daily, more in the afternoon and night. During these episodes she had a miserable look and some chills but no skin rashes. In between she was feeling good and with normal activity. Fundoscopy done eight days after admission showed disseminated choroidal tubercles as shown in (Fig. 2). At this point she was started on 4 anti tuberculous drugs (Isoniazid, Rifampin, Streptomycin and Pyrazinamide) and Prednisolone. Within one week the ascites disappeared on ultrasound and within the next week fever disappeared and liver edge was shrunken to 5 cm below costal margin. Within 2 months liver span and chest x-ray was nearly normal. Four weeks after admission the culture of all three fasting gastric aspirates grew Mycobacterium tuberculosis. Screening of the whole family members by PPD and chest x-rays were negatives.
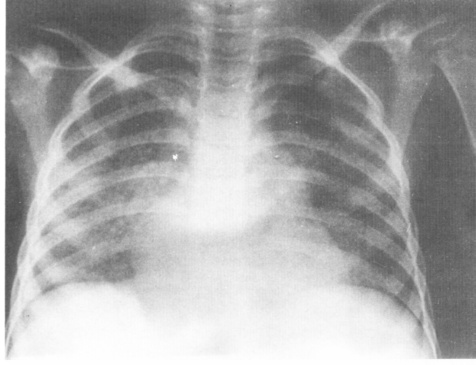 Fig. 1:
Fig. 1:Chest X-ray showed diffuse miliary shadowing bilateral.
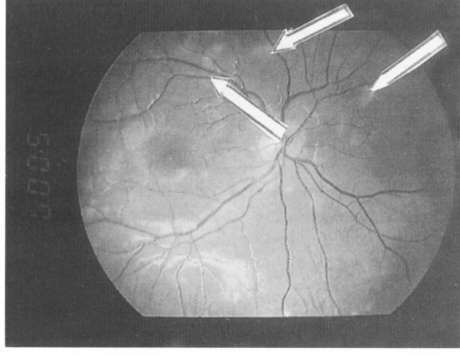 Fig. 2:
Fig. 2:Disseminated choroidal tubercles.
Discussion
Our patient presented with a longstanding history of fever and weight loss. Clinical examination revealed gross hepatomegaly, choroidal tubercle, and remitting fever. Clinically she was not ill except during the spikes of fever where she used to set or lie in bed shivering.
Disseminated TB usually occurs because of the inadequacy of the host defense in containing the infection (3). Multiorgan involvement is probably much more common than recognized because, generally, once Mycobacterium tuberculosis is isolated in any specimen other sites are usually not evaluated. Patients with this disease usually have ill looking, in contrast to our patient who was feeling good between the spikes of fever.
The presenting symptoms and signs of disseminated tuberculosis are generally nonspecific and dominated by systemic effects particularly fever, weight loss and night sweats (2-5). Fever itself constitutes the most frequent symptom in disseminated tuberculosis, and it might be of long duration (2-4). In Gurkan et al series fever reported in 74% and the duration of onset of symptoms prior to admission ranged between 15 days and 8 months (4). It was found in nearly all the patients reported by Rahajoe (2). Other symptoms of disseminated tuberculosis depend on the relative severity of disease in the organ involved.
Although productive cough was reported as the most frequent symptom in some series (5), our patient denied any history of cough despite a wide spread of nodular shadows in the lungs. Even more there was no localized physical finding in her chest. This emphasizes the importance of chest radiography in cases of prolonged fever even in the absence of respiratory symptoms.
Chest film is usually abnormal in most but not all patients with disseminated tuberculosis. In the series reported by Hussey et al, 85 of 94 patients (94%) had classic miliary pattern (5), whereas almost all children reported by Guken et al had miliary shadows in chest films (4). Chest x-ray taken in our patient one month prior to admission reported as a normal in contrast to the one taken during admission. It is not yet known how long it takes to have the classic miliary shadows in the chest film from the beginning of the disease.
This might explain absence of these finding in patients reported in some articles (5). It may be that patients diagnosed early the disease might not have the typical miliary shadows in the chest x-rays. Or it might be that not all patients with disseminated tuberculosis had chest x-ray taken because of scanty respiratory symptom as in our case.
Physical findings are variable; hepatomegaly, splenomegaly, and lymphadenopathy are found in decreasing frequency (2,5). In our patient in addition to gross hepatomegaly there was some pelvic ascites, but there was no enlarged lymph nodes. Unfortunately, we were not able to know the nature of the pelvic ascites. The hepatomegaly is mostly due to tuberculous hepatitis, which might explain the liver enzymes leak in our case.
A finding that is always strongly suggestive of disseminated tuberculosis is the choroidal tubercles, a granuloma located in the choroid (6).
They occur in 13% -87% of patients (7). These tubercles that found in our patients made us start treatment before the culture results. In the presence of these findings treatment should be commenced soon after taking suitable accessible samples for culture particularly in developing countries where fast laboratory tests are unavailable. Interestingly our patient denied any visual or eye complains in spite of the disseminated choroidal tubercles in both eyes.
Fernandes et al reported two cases of miliary tuberculosis with choroidal tubercles (8). They stressed the importance of the combination of clinical findings and the presence of choroidal tubercles in the final diagnosis and correct treatment. The ophthalmoscopic form of tuberculosis usually consists of nodules or tubercles that are grayish or white, have indistinct borders, and vary in size from one-sixth to two third of papillary diameter (8-11). The lesions are hypoflourescent initially, and then show a hyper-fluorescence that increases in size. They leave a scar with or without pigmentation.
To our knowledge there was no reports on the disseminated choroidal tubercles in miliary tuberculosis from the Royal Medical Services hospitals
Our patient was not vaccinated with BCG. Although the efficacy of this vaccine is uncertain, there are ample data indicating that BCG vaccine protects against disseminated tuberculosis and tuberculous meningitis (12).
Reporting this case in Jordan might justify the national policy regarding BCG vaccine according to the new EPI program (40 days) instead of the 6-years age.
In conclusion tuberculosis should always be in the differential list in patients with questionable diagnosis. Patients with disseminated tuberculosis might have neither respiratory symptoms nor signs.
References1.
Vijayan VK. Disseminated tuberculosis. J Indian Med Assoc. 2000; 98(3): 107-109.
2.
Rahjoe NN. Miliary tuberculosis in children. A clinical review. Pediatr Tndones 1990; 30(9-10): 233-240.
3.
American Thoracic Society. Diagnostic standards and classification of Tuberculosis in adults and children. Am J Resir Care MED 2000; 161: 1376-1395.
4.
Gurkan F, Bosnak M, Dikici B, et al. Miliary tuberculosis in children: A clinical review. Scan J Infect Dis 1998; 30(4): 359-362.
5.
Hussey G, Chisholm T, Kibel M. Miliary tuberculosis in children a review of 94 cases. Pediatr Infect Dis J 1991;10(11): 832-835.
6.
Massaro D, Kats S, Sachs M. Choroidal tubercles: A clue to hematogenous tuberculosis. Ann Intern Med 1964; 60: 231-241.
7.
Starke JR, Munoz F. Mycobacterial Infections. In: Behrman R, Kliegman R, Jenson H. Nelson Textbook of Pediatrics 16th Edition. WB Saunders Company, London. 2000; 6: 885-886.
8.
Fernandes CC, Gacia JJ, Moro BD, et al. Choroidal tubercles in miliary tuberculosis. Arch Soc Esp Otalmol 2000; 75(5): 355-358.
9.
Yago K, Takahashi M. A case of miliary tuberculosis. Folia Ophthalmol Jpn 1976; 27: 1172-1176.
10.
Kiyosawa R, Ohnishi K, Ikeda T. A case of miliary tuberculosis. Folia Ophthalmol J pn 1985; 36: 652-656.
11.
Takishi shiono, Shi-ichi A, Toshio H. A case of miliary tuberculosis with disseminated choroidal hemorrhages. British J of Ophthalmology 1990; 74: 317-319.
12.
Shapiro C, Cook N, Evans D, et al. A case-control study of BCG and childhood tuberculosis in Cali, Colombia. Int J Epidemiol 1985; 14: 441-446.