Objective: Technetium-99m red blood cell scintigraphy is a very specific method to differentiate a haemangioma from other hepatic masses. The purpose of this study is to evaluate the efficacy of planar scintigraphy and single photon emission computed tomography Technetium-99m-labeled red blood cell in the investigation of suspected hepatic cavernous hemangioma.
Methods: The study group consisted of one hundred and five patients, 62 females (59%) and 43 males (41%), between 23-69 years of age (mean age of 41). These patients were evaluated for liver masses found on ultrasound. The final diagnosis was made after liver biopsy or aspiration cytology in 26 patients and after follow-up, by maintaining stable clinical course ranging for one year with no changes in the size or appearance of the lesion on ultrasound in 79 patients.
Results: One hundred and thirty two lesions were found; haemangioma in 96 patients and non-hemangiomatous lesions in 36 patients. Planar 99m Tc- red blood cell showed sensitivity and specificity of 67% and 100% respectively, while, 99mTc-red blood cell- single photon emission computed tomography showed sensitivity and specificity of 81%, 97%, respectively. The use of single photon emission computed tomography showed better sensitivity value than PS from hemangiomas < 2.5 cm (61% for single photon emission computed tomography versus 24% for planar scintigraphy).
Conclusion: Tc-99m RBC scintigraphy is a simple, noninvasive and accurate technique in the detection of hepatic hemangioma. It can distinguish hemangioma from other hepatic lesions. single photon emission computed tomography is superior to planner imaging in the detection of small hemangioma and should be performed whenever planar imaging fails to show the lesion by 2 hours. Lesions less than 1.1 cm cannot be detected by Tc-99m red blood cell single photon emission computed tomography because they are beyond the limit of spatial resolution of the gamma camera used.
Key word: Liver, Hemangioma, 99mTc-RBC, SPECT.
JRMS June 2006; 13(1): 9-14IntroductionHemangioma is the most common benign hepatic tumor (1-3) and second most common neoplasm of the liver, following intrahepatic metastases(4). Usually, they occur as a solitary lesion, however, they may be multiple in 10% of patients (5). It occurrence in the general population is around (1-20%) (1,2,6-10), and it is more common in females than males (2,7).
Because hepatic hemangiomas are frequent, most often asymptomatic and have a very low rate of complications (2,8,-11), this lesion does not require surgical resection (1,9,12). Therefore, the role of imaging is to diagnose the lesion, thus avoiding an unnecessary invasive procedure (5).
The imaging features of a hemangioma depend on its size (6); typical hemangiomas are mostly less than 3 cm in diameter. Most hemangiomas remain stable in size (3,8) or demonstrate minimal increase in diameter over time (2,3).
In cases of typical hemangioma, imaging modalities like magnetic resonance imaging (MRI) (3,8,13-17), computerized tomography (CT) (3,8,10,18,19) scan and ultrasound (US) (2,9,20-24,) are highly reliable for diagnosis.
Although atypical hemangiomas are rare, many radiologists will encounter atypical findings (3) due to the high prevalence of hepatic hemangiomas (2).
This may lead to misdiagnosis and confusion with other lesions (3). In some cases, a specific diagnosis can be established with imaging, modalities, however, in other atypical cases, the diagnosis will remain uncertain at imaging, and may require histopathologic examination (6).
Nuclear medicine imaging techniques continue to play a unique role in the evaluation of hepatic masses (1,4,12). Although many useful radiodiagnostic agents are available (4), the predominant nuclear medicine study used to evaluate hepatic masses is technetium-labeled red blood cell (RBC) "blood-pool" scintigraphy (4,7,14,25-31). Hepatic blood-pool scintigraphy is extremely useful for the confirmation or exclusion of benign hepatic hemangiomas (4,12,14,26-31). With this method, there is decreased activity on early dynamic images and increased activity on delayed blood pool images obtained over 30–50 minutes (7,26). All hemangiomas showed various presentations of the perfusion blood pool mismatch, which is the basis for diagnosis (26-29). The sensitivity and specificity of blood-pool scanning for the detection of hemangiomas has continued to improve over the years (7,26).
This improvement has been caused predominantly by advancements in instrumentation; especially the development of single photon emission computed tomography (SPECT) imaging (4,7,25,27,28,30). Numerous studies have demonstrated that the sensitivity of single photon emission CT is superior to that of planar imaging (7,30).
This study was carried out to demonstrate the most important advantages of 99mTc-blood pool SPECT versus the established method of planar scintigraphy (PS) in the non-invasive diagnosis of liver hemangiomas.
Methods
PatientsThe study was conducted at King Hussein Medical Center (KHMC) during the period between March 2002 and August 2003. One hundred and five patients, 62 females (59%) and 43 males (41%), between 23-69 years of age (mean age of 41) were included in this study. These patients were referred to nuclear medicine department after the incidental finding of a solid liver mass/s found on ultrasonography. The final diagnosis was made after liver biopsy and aspiration cytology in 26 patients and by maintaining a stable clinical course with no change in the size and shape of the lesion, for 6-12 months, by ultrasonography in 79 patients.
Scintigraphy with 99mTc-Labeled RBC Scintigraphy was performed using in vivo method for labeling red blood cells with 99mTc-pertechnitate. Patients were injected intravenously with 20 μg stannous per Kg of body weight. After 20 min, patients were positioned over the table of a double head GE Millenium gamma camera in the supine position with liver and spleen centered in the field of view. The patients were injected intravenously with 20-30 mCi of 99mTc-pertechnitate.
Planner ImagingAnterior dynamic planner imaging, for the liver area, was started immediately after the injection. The imaging sequence was as follows: a 2-second frame for 2 min to assess blood flow to the liver followed by a 30-second frame for 45 minutes. A delayed static Planner images at 2 hours post injection were performed with 128 x 128 image matrix, a 10% window and an energy peak of 140 (KeV). For each patient, an anterior, posterior, and both lateral views were taken for the liver area, each with 700, 000 counts. A low-energy high-resolution collimated gamma camera without zoom was used. The camera was positioned as close as possible to the patients.
SPECT ImagesSingle photon emission tomography imaging was performed after the second planner images, 2 hours post injection. Acquisition protocol includes the use of an elliptical orbit, 360o, 64 emission (20-30 second per emission) and we use a 128 x 128 image matrix with 1.4-1.5 magnification. Images were processed using a commercial software program (G Entegra), in the transverse, sagital and coronal slices; using butterworth filter with 0.3 cutoff or Hanning with 0.8-cutoff and slices thickness 6-12mm.
Images AssessmentTwo readers assessed each set of images. When the two readers disagree; a third reader will decide which study represent a positive results for haemangioma. We defined a 'focal positive study' when we observed one or more clearly defined areas of abnormal increase trace uptake in relation to the surrounding tissue, placed in the liver area; visible in delayed planner or SPECT images, not seen in the early images. The study was 'negative' when it did not correspond to the previous situation (29,35).
Methods of AnalysisSensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were decided in the traditional methods.
Results The study group includes 105 patients; 62 females (59%) and 43 males (41%).
Ultrasonic ResultsOne hundred and thirty two lesions were found. The sizes of the lesions ranged from 0.5 to 9 cm. With regard to the distribution of the lesions, 88 (84%) Patients had single lesions; and 17 (16%) patients had multiple lesions. One hundred and twenty (91%) lesions were in the right lobe and 12 (9%) lesions in the left lobe.
Pathological ResultsHemangiomas were fond in 96 lesions and non-hemangiomatous lesion in the remainder which includes; hepatocellular carcinoma, focal nodular hyperplasia, simple cysts and metastasis. Four patients had more than one hemangioma in their liver (Fig. 1).
99m Tc-RBC planners Scintigraphy (PS) Tc-99m RBC planner Scintigraphy (Table I and II) was truly positive in 64 out of 96 lesions and false negative in the remainder 32 hemangiomatous lesions. There was no false positive in any non-haemangiomatous lesion. For lesions ≥ 2.5 cm 56 out of 63 lesions were detected, while only 8 out of 33 lesions < 2.5 cm were detected by PS. The smallest lesion detected by PS was 1.8 cm.
99m Tc-RBC SPECT Scintigraphy (SPECT RBC) (Table I)
SPECT (Table I and II) was positive in 83/96 and negative in 13/96 haemangiomatous lesions. There was one false positive result in non-haemangiomatous lesions. All lesion ≥ 2.5 cm were detected by SPECT RBC while 20/33 lesion < 2.5 cm were detected by SPECT RBC. The smallest lesion detected by SPECT RBC was 1.1 cm. SPECT scan diagnosed 2 hemangiomatous lesions not diagnosed by US in patients with cirrhotic liver.
Discussion
Hepatic hemangiomas are frequent and usually discovered incidentally during an US or CT scan examination of the abdomen (22,2).
Typical hemangiomas are mostly less than 3 cm in diameter (3). Large hemangiomas are often termed giant hemangiomas when they exceed 4 cm in diameter (2,33,34). However, some authors define giant hemangiomas as lesions greater than 6-cm (1,25) or 12 cm in diameter (35,36).
Hemangiomas are most often asymptomatic (1,2). Complications are mostly observed in large hemangiomas (1,5,11,37) and can be divided into alterations of internal architecture (37), coagulopathy (1,5), and inflammation; hemorrhage (11,38), which can cause hemoperitoneum (38); volvulus; arterioportal venous shunting (27,10) and compression of adjacent structures (38,37,1).
The clinical importance of these tumors relates to distinguishing them from malignancy. Therefore, the role of imaging is to help diagnose the lesion.
The most commonly used imaging modalities to evaluate hemangiomas are US (2,9,20,21,24,34), CT (8,10,18,19,34), MRI (8,15-17) and technetium-99m labeled red blood cell planer and single photon emission computed tomography (Tc-99m RBC SPECT).
The typical appearance by US is a homogeneous, echogenic mass with well-defined margins (2). However, this appearance is non-specific (2,20-22) and can also be seen in adenomas, hepatocellular carcinomas, and metastatic disease (9,23,34) or cannot be seen in patients with cirrhotic liver (2,3,32) or giant hemangioma (25). The CT scan findings consist of a low attenuating lesion on nonenhanced images following intravenous administration of contrast material; peripheral puddling of contrast is seen (8,10,22). The classic findings are not always evident (2,6,18,19,34) or can be seen with other lesion (39).
At MR imaging, hemangiomas are characterized by well-defined margins and high signal intensity on T2-weighted images as the time to echo (TE) is lengthened, and demonstrates peripheral puddling of contrast on the enhanced images (8,16,17). Approximately 5% of malignant tumors mimic hemangiomas on these long TE images, which reduce the specificity of MRI for hemangiomas (13,40). Its sensitivity is relatively low for small hemangiomas (16), but may be better than Tc-99m RBC SPECT.
Tc-99m RBC SPECT scintigraphy is extremely useful for the confirmation or exclusion of benign hepatic hemangiomas (4,7,14,25-30,34). With this method, there is decreased activity on early dynamic images following injection of radioactive material, and increased activity (Mismatch Pattern) on delayed blood pool images obtained over 30–50 minutes (7,29). Numerous studies have demonstrated that the sensitivity of single photon emission CT is superior to that of planar imaging (7,30)
Our results for planer scintigraphy with 99mTc-RBC showed an overall sensitivity, specificity, and positive and negative predictive values of 67%, 100%, 100% and 53%, respectively, while SPECT 99mTc-RBC showed an overall sensitivity, specificity, and positive and negative predictive values of 86%, 97%, 99%, and 70% respectively. The use of SPECT improved the overall sensitivity by 19%.
SPECT demonstrated 19 hemangiomas that were not detected with planner imaging (Fig 2) 12 of them were smaller than 2.5 cm. Planar imaging alone would have missed these lesions.
When the hemangioma size was ≥ 2.5 cm; the sensitivity of SPECT was 100% while for planer images, the sensitivity was 89%, which is still relatively high. When hemangiomas confined to nodules smaller than 2.5 cm in diameter; 24% of hemangiomas were detected by planar delayed RBC imaging. With the addition of SPECT, the sensitivity in the detection of hemangiomas less than 2.5 cm, was improved by 37% (61% versus 24%).
The smallest hemangioma shown by delayed RBC-SPECT scanning was 1.1 cm in diameter, compared with 1.8 cm by planar RBC scanning.
Scintigraphic diagnosis of a liver hemangioma may be difficult when its size approaches the spatial resolution of a gamma camera, and it may not be visualized on a Tc-99m RBC planer and SPECT studies. This was obvious with the decrease in the sensitivity for lesion less than 2.5 cm and with non-visualization of lesion less than 1.2 cm.
When confronted with clinical data and a preliminary radiologic study suggestive of hemangioma, serial planar blood-pool scintigraphy (with SPECT if the lesion is < 3-4 cm) should probably be the initial diagnostic examination. Due to its high specificity, when the suspected hepatic hemangioma is confirmed by a positive radionuclide blood-pool study, the clinical evaluation of patients with hepatic masses can generally be terminated.
False positive results had been described in literature (41-43). In our study there was one false positive lesion seen by SPECT, which was not seen neither by PS nor by US. False negative results in large hemangioma were also reported in the literature but not in our study (34,44,45).
The SPECT approach is considered superior to planar blood pool imaging because of improved diagnostic yield reduced patient imaging time, and greater ease of correlation with other cross-sectional imaging modalities. SPECT allowed a correct visualization of abdominal and intrahepatic major vessels.
In comparison to MRI, 99mTc-RBC SPECT is safer, less expensive, and easier for some patients to tolerate and is more specific although less sensitive especially with small lesion. Its major advantage over computed tomography scan is its safe application in cases with contrast agent intolerance and hyperthyroid patients. Moreover, liver biopsies are dangerous and ill suited for the verification of diagnosis. However, fine-needle biopsy is more useful for confirming a suspected malignancy than for actually diagnosing hemangioma.
The use of ultrasound should precede scintigraphy for two important reasons; first of all most of these patients are discovered incidentally during ultrasound examination and secondly; the size and the location of the lesion (anterior or posterior) is important for optimal gamma camera acquisition parameters.
99mTc-labeled red blood cell (RBC) scanning is considered a highly specific technique for the study of hepatic hemangiomas. However, planar imaging displays poor sensitivity for the identification of small lesions.
Conclusion
This study suggests that SPECT-RBC of the liver is the nuclear medicine study of choice in the diagnosis of hepatic hemangioma. It is useful for differentiating hemangioma from other liver tumors. Due to its high specificity, the clinical evaluation of patients with hepatic masses can generally be terminated when it is positive.
It has a considerably higher sensitivity than planar imaging in the detection of hemangiomas, and greater ease of correlation with other cross-sectional imaging modalities.
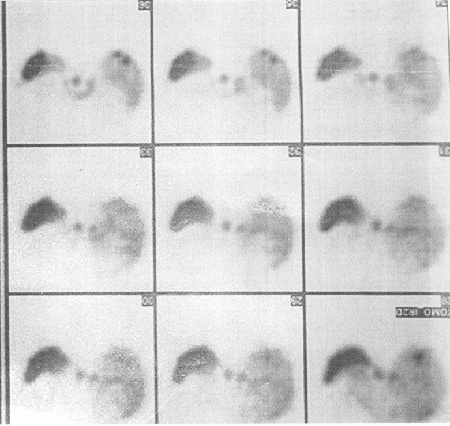 Fig. 1:
Fig. 1:Patients with two hemangiomas in the right lobe of the liver.
Table I:The results of planner and SPECT labeled RBC Scintigraphy.
|
Us (Total=132)
|
SPECT
|
PS
|
|
a. Hemangioma
|
+
|
-
|
+
|
-
|
|
≥2.5 cm
|
63
|
63
|
100%
|
0
|
0%
|
56
|
89%
|
7
|
11%
|
|
<2.5 cm
|
33
|
20
|
61%
|
13
|
39%
|
8
|
24%
|
25
|
76%
|
|
Total
|
96
|
83
|
86%
|
13
|
14%
|
64
|
67%
|
32
|
33%
|
|
b.
Non-hemangioma
|
+
|
-
|
+
|
-
|
|
Total
|
36
|
1
|
3%
|
35
|
97%
|
0
|
0%
|
36
|
100%
|
Table II: The results of sensitivity, specificity, PPV and NPP for both PS and SPECT.
|
|
SPECT
|
PS
|
|
Sensitivity
|
86%
|
67%
|
|
Specificity
|
97%
|
100%
|
|
PPV
|
99%
|
100%
|
|
NPV
|
70%
|
53%
|
References 1.
Beckingham IJ, Krige JEJ. ABC of diseases of liver, pancreas, and biliary system (Liver tumors). BMJ 2001; 322: 477-480.
2.
Avva R, Shah HR, Angtuaco TL. US Case of the day. Radiographics. 1999; 19:1689-1692.
3.
Yu J-k, Kim KW, Park MS, Yoon S. Hepatic Cavernous Hemangioma in Cirrhotic Liver: Imaging Findings. Korean Journal of Radiology 2000 December; 1(4): 185-190.
4.
Krausz Y, Levy M, Antebi E, et al. Liver Hemangioma: A Perioperative Tc-99m RBC SPECT Correlation. Clin Nucl Med 1997; 22(1): 35-37.
5.
Narayanan G, Yang DC, Tai KG, et al. Giant Hepatic Hemangioma Studied With Intravenous Total Body Arteriography Technique: A Case Report. Clin Nucl Med 1996; 21(6): 456-459.
6.
Brancatelli G, Federle MP, Blachar A, Grazioli L. Hemangioma in the Cirrhotic Liver: Diagnosis and Natural History. Radiology 2001; 219: 69-74.
7.
El-DesoukI M, Mohamadiyeh M, Al-Rashed R, et al. Features of Hepatic Cavernous Hemangioma on Planar and SPECT Tc-99m-Labeled Red Blood Cell Scintigraphy. Clin Nucl Med 1999; 24(8): 583-589.
8.
Horton KM, Bluemke DA, Hruban RH, et al. CT and MR Imaging of Benign Hepatic and Biliary Tumors. Radiographics 1999; 19:431-451.
9.
Leifer DM, Middleton WD, Teefey SA, et al. Follow-up of Patients at Low Risk for Hepatic Malignancy with a Characteristic Hemangioma at US. Radiology. 2000; 214: 167-172.
10.
Kim KW, Kim TK, Han JK, et al. Hepatic Hemangiomas with Arterioportal Shunt: Findings at Two-Phase CT Radiology. 2001; 219:707-711.
11.
Cappellani A, Zanghi A, Di Vita M, et al. Spontaneous rupture of a giant hemangioma of the liver. Ann Ital chir 2000; 71(3): 379-83. (Abstract)
12.
Rubin RA, Lichtenstein GR. Scintigraphic evaluation of liver masses: cavernous hepatic hemangioma. J Nucl Med 1993: 34(5) 849-852, (abstract)
13.
Keogan MT, Edelman RR. Technologic Advances in Abdominal MR Imaging. Radiology. 2001; 220:310-320
14.
Brown RK, Gomes A, King W, et al. Hepatic hemangiomas: evaluation by magnetic resonance imaging and technetium-99m red blood cell scintigraphy. J Nucl Med 1987; 11(28): 1683-1687 (abstract)
15.
Jeong M-G, Yu J-S, Kim K W. Hepatic Cavernous Hemangioma: Temporal Peritumoral Enhancement during Multiphase Dynamic MR Imaging. Radiology. 2000; 216: 692-697.
16.
U¨nala O, Sakaryaa E, Arslana H, et al. Hepatic cavernous hemangiomas. Patterns of contrast enhancement on MR fluoroscopy imaging. Journal of Clinical Imaging 2002; 26: 39-42.
17.
Li CS, Chen RC, Chen WT, et al. Temporal Peritumoral Enhancement of Hepatic Cavernous Hemangioma. Findings at Multiphase Dynamic Magnetic Resonance Imaging. J Comput Assist Tomogr 2003; 27: 854-859.
18.
Kim T, Federle MP, Baron RL, et al. Discrimination of Small Hepatic Hemangiomas from Hypervascular Malignant Tumors Smaller than 3 cm with Three-Phase Helical CT. Radiology. 2001; 219: 699-706.
19.
Blachar A, Federle MP, Ferris JV, et al. Radiologists’ Performance in the Diagnosis of Liver Tumors with Central Scars by Using Specific CT Criteria. Radiology 2002; 223: 532-539.
20.
Sommer G, Olcott EW, Tai L. Liver Tumors: Utility of Characterization at Dual-Frequency US Radiology. 1999; 211: 629-636.
21.
Wilson SR, Burns PN, Muradali D, et al. Harmonic Hepatic US with Microbubble Contrast Agent: Initial Experience Showing Improved Characterization of Hemangioma, Hepatocellular Carcinoma, and Metastasis. Radiology. 2000; 215: 153-161.
22.
LEe JY, Choi BI, Han JK, et al. Improved Sonographic imaging of hepatic hemangioma with contrast-enhanced coded harmonic angiography: comparison with MR imaging. Ultrasound in Med. & Biol 2002; 3(28): 287-295.
23.
Blomley MJ, Sidhu PS, Cosgrove DO, et al. Do Different Types of Liver Lesions Differ in Their Uptake of the Microbubble Contrast Agent SH U 508A in the Late Liver Phase? Early Experience. Radiology. 2001; 220: 661-667
24.
Isozaki T, Numata K, Kiba T, et al. Differential Diagnosis of Hepatic Tumors by Using Contrast Enhancement Patterns at US. Radiology 2003; 229: 798-805.
25.
Csai CT, Yen TC, Tzen KY. The Value of Tc-99m Red Blood Cell SPECT in Differentiating Giant Cavernous Hemangioma of the Liver from Other Liver Solid Masses. Clin Nucl Med, 2002; 27(8): 578-581.
26.
Mernagh JR, Skehan S, Thompson M, et al. Nuclear Medicine Examination of the Gastrointestinal Tract. The Radiologist 2002; 4(9): 165-185.
27.
Dwamena BA, Belcher KK, Dasika N, et al. Focal Hyperemia on RBC Blood-Flow Imaging: A Scintigraphic Marker of Arterioportal Venous Shunting in Hepatic Cavernous Hemangiomas? Clin Nucl Med 1997; 22(8): 542-545.
28.
Schillaci O, Danieli R , Manni C , et al. Technetium-99m-labelled red blood cell imaging in the diagnosis of hepatic haemangiomas: the role of SPECT/CT with a hybrid camera. Eu J Nucl Med and Mol Ima 2004; 31: 1518-1519
29.
Royal HD, Israel O, Parker JA, Kolodny GM. Scintigraphy of hepatic hemangiomas: the value of Tc-99m-labeled red blood cells: concise communication J Nucl Med, 1981; 22(8): 684-687. (Abstract)
30.
Wang J, Slizofski W, K Russell, et al. The Changing "Face" of 99mTc-labeled RBC Imaging and Hepatic Hemangioma. Clin Nucl Med. 1996; 21(4): 348.
31.
Taylor RER. Tc-99m-Labeled Red Blood Cell Scan Showing Gastrointestinal Bleeding Point, and Also Showing an Incidental Hepatic Hemangioma. Clin Nucl Med 2004; 29: 211-213.
32.
Caturelli E, Pompili M, Bartolucci F, et al. Hemangioma-like Lesions in Chronic Liver Disease: Diagnostic Evaluation in Patients. Radiology. 2001; 220: 337-342.
33.
Nghiem HV, Bogost GA, Ryan JA, et al. Cavernous hemangiomas of the liver: enlargement over time. AJR 1997; 169: 137-140.
34.
Demirtürk L, Yazgan Y, Ozel MA, Narin Y. Giant hepatic hemangioma mimicking hepatocellular carcinoma. (Letters to the Editor). Journal of Gastroenterology and Hepatology 2003; 18: 112-117.
35.
Kaido T, Imamura M. Giant Hepatic Hemangioma. N Engl J Med 2003; 349(20) 167-172.
36.
Landor M, Petrozzo P. Images in clinical medicine (Hepatic Hemangioma). The N Engl J Med 2001; 342(11) 791-792.
37.
Cortés-Blanco A, MartíneZ-Lázaro R. Bile duct stenosis seemingly caused by a giant pedunculated hemangioma with hypogastric growth interesting images. Clin Nucl Med 2000; 25(4): 299-300.
38.
Casillas VJ, Amendola MA, Gascue A, et al. Imaging of nontraumatic hemorrhagic hepatic lesion. Radiographics. 2000; 20: 367-378.
39.
Nino-Murcia M, Olcott EW, Jeffrey RB, et al. Focal liver lesions: pattern-based classification scheme for enhancement at arterial phase CT Radiology 2000; 215: 746-751.
40.
Jeong YY, Mitchell DG, Holland GA. Liver lesion conspicuity: T2-weighted breath-hold fast spin-echo MR imaging before and after gadolinium enhancement-initial experience Radiology 2001; 219: 455-460.
41.
Eun-kyung JI, Ryu JS, Kang GH, et al. Pelioid-type hepatocellular carcinoma masquerading as a hepatic hemangioma on technetium-99m red blood cell scintigraphy. Clin Nucl Med 2001; 26(1): 33-35.
42.
Lim ST, Sohn MH. A case of hepatocellular carcinoma mimicking cavernous hemangioma on Tc-99m RBC liver SPECT. Clin Nucl Med 2001; 26(3): 253-254.
43.
Shih WJ, Lee JK, Mitchell B. False-positive results for hepatic hemangioma on Tc-99m RBC SPECT caused by a liver metastasis from small-cell lung carcinoma. Clin Nucl Med, 1996; 21(11): 898-899.
44.
Decorato D, Finestone H, Horowitz M. Lack of uptake of tagged erythrocytes in a large hepatic hemangioma [Interesting Images]. Clin Nucl Med. 1999; 24(8): 606-608.
45.
Larcos G, Farlow DC, Gruenewald SM, Antico VF. Atypical appearance of an hepatic hemangioma with technetium-99m red blood cell scintigraphy. J Nucl Med 1989; 30(11): 1885-1888.