Objective: To report our initial experience in evaluating the role of 16-slice multidetector computed tomography (MDCT) in the non-invasive detection of coronary artery disease.
Methods: During a period of three months (between 15/12/2004 to 21/3/2005), 50 patients (39 M, 11 F; mean age 54 ±7.2 years) in sinus rhythm with stable angina pectoris scheduled for conventional coronary angiography, were examined with a 16-slice multidetector computed tomography (GE Medical systems, USA) which began working at King Hussein Medical Center at mid 2004. Multiplanar reconstructions were made for all coronary artery segments with a diameter above 2mm. A total of 14 coronary vessel segments were assessed in each patient with respect to image quality, presence and degree of coronary artery stenosis and the amount of coronary artery calcification.
Results: Six hundred sixty three segments were studied (there were 46 significant lesions). The images were classified as good, adequate and poor in 584 (88%), 37(5%) and 42(7%) segments respectively. The sensitivity, specificity, positive and negative predictive value of MDCT for the detection of significant lesions were 82%, 97%, 71% and 98% respectively. False negative results occurred in 10 segments, 6 of which were in the left circumflex coronary artery branch and mid right coronary artery. The false positive segments were 19, 74% of these (n=14) were calcified.
Conclusion: Multidetector computed tomography is sensitive and highly specific in the detection of coronary artery disease in patients with stable angina. It is expected that using the new generation of 64-row scanners will get better results.
Key words: Coronary artery disease, Multidetector computed tomography, Stable angina.
JRMS April 2007; 14(1): 5-12
IntroductionFor nearly 50 years, invasive conventional coronary arteriography (CCA) has been the reference standard for defining epicardial coronary artery disease (CAD). Unfortunately, CCA is not without risk (0.15% mortality and 1.5% morbidity rates(1)) or inconvenience for the patient and the search continues for an alternative, noninvasive method to detect and assess the severity of CAD.
Multidetector computerized tomography (MDCT) with simultaneous acquisition of four slices has become available since 1999. Initial experiences have suggested that CAD can be detected with good sensitivity and specificity(2-5).
The resolution of the MDCT continued to improve with the advent of the 16 row scanners that acquire thinner slices and rotate faster. Three–dimensional volume-rendered and multiplanar images display arterial anatomy similarly to CCA. Use of these two techniques gave higher sensitivity. Well-planned clinical trials using this technology showed extremely improved results(6,7) and lower number of unassessable vessels (7% vs. 27%) in comparison to the four slice generation scanners(8).
The sixteen rows MDCT has become available at King Hussein Medical Center (KHMC) in mid 2004. Since these scanners have the potential to allow noninvasive coronary angiography, we aimed to investigate this potential value in a group of patients with stable angina who were referred to Queen Alia Heart Institute (QAHI) for assessment of their CAD. To our knowledge this is the first report in our region to address this important emerging issue.
Methods
During a period of 3 months, we studied 50 patients (39 men, 11 women, mean age 54 ±7.2 years) who were admitted to QAHI with stable angina pectoris and were scheduled for MDCT that was performed within two weeks before CCA, in order to determine the presence and extent of coronary artery disease.
The patients were placed within the gantry of a 16-row MDCT scanner (Light SpeedTM 4.0, GE Medical Systems, USA). The scan parameters were: 16 x 0.625 mm collimation; tube rotation time 500 ms; tube voltage 100 kV; tube current 420 mAs. No tube modulation was used. Patients with a heart rate above 70 beats/min received a single oral dose of 50-200 metoprolol 1-2 hours before the scan unless contraindicated (overt heart failure or severely compromised pulmonary function).
By using a single head power injector (Medrad, Vistron CT, USA) a bolus of 120 ml contrast material with iodine content of 370 mg/ml (Iopamiro®, Bracco -s.p.a. Milano, Italy) was injected through an arm vein at a flow rate of 4 ml/sec. Data were acquired during a breathhold of 20 seconds and were sent to a separate workstation (ADW 4.0, GE, USA) that was used to reconstruct the images using the standard built-in retrospective ECG-dependent reconstruction algorithms during mid-to-end diastole in order to obtain motion-free images.
These algorithms improve the temporal resolution and reduce the effective slice thickness at an acceptable increase in noise and reduction in contrast. Datasets of a single heartbeat were obtained during half a rotation time resulting in a temporal resolution of about 190ms. Transaxial images were reconstructed in 0.5mm increments with an effective slice thickness of 0.625mm.
Exclusion criteria were patients with irregular rhythm, those unable to perform a 20sec breath-hold, those presenting with acute coronary syndrome or have contraindications to iodinated contrast material. Patient characteristics are summarized in Table I where variables are expressed with their mean + standard deviation and categorical data are presented with absolute numbers and percentages.
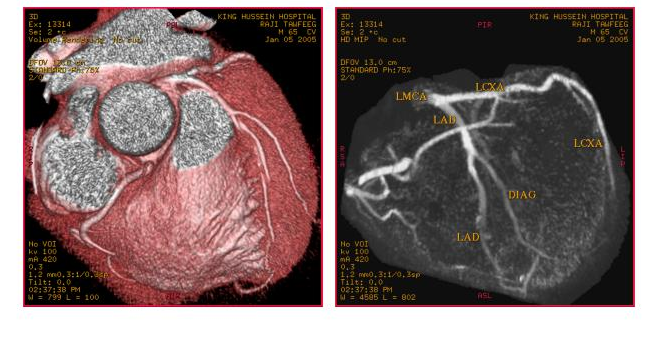
All scans were analyzed by one observer blind to the results of conventional coronary angiography and 0.625 mm maximum intensity projections as well as three dimensional volume rendering images were used to detect and identify severity of coronary lesions (Fig 1 & 2).
Lesions were classified as significant or non-significant according to a modified American College of Cardiology/American Heart Association classification (ACC/AHA) in a joint reading(9). However, minor further modifications were done assigning three segments (proximal, mid and distal) for the left main coronary artery because of its great importance.
Diagonal arteries were assigned one segment only instead of two. Left anterior descending artery (LAD), left circumflex artery (CX) and right coronary artery (RCA) segments were assigned exactly according to the mentioned modification. Therefore, 14 segments in each patient (3 for LM, 3 for LAD, 1 for the DL, 3 for CX and 4 for RCA) were identified and analyzed. The total number of studied segments was 663 segments ({50x14} - 37) for the whole study group.
Segments that were excluded were: Stented segments (n=4), occluded segments that do not fill late in conventional angiography (n=14), segments that could not be assessed (n=8), very short segments (n=1) happened in the mid left main and both distal and branch RCA segments when the vessel is nondominant on conventional angiography (n=10). The total number of excluded segments was therefore 37 segments.
Coronary vessel segments were assessed in each patient with respect to image quality (good, adequate and poor), percentage of coronary artery narrowing, and the amount of coronary artery calcification (0=non, 1=mild to moderate, 2= severe). The definitions of image quality and amount of calcification are shown in Table II.
Image quality was classified as poor in 42 (7%) of the segments. However these segments were included in the comparative analysis with QCA. Conventional coronary angiograms were done according to the standard techniques and were evaluated by quantitative coronary analysis (QCA, Philips Medical Systems, and Netherlands) with automated vessel contour detection. Stenoses were evaluated in two orthogonal views by one cardiologist blinded to the MDCT results, and they were classified as significant if the mean lumen diameter reduction was ≥ 50%. All segments ≥ 2mm were included for comparison with MDCT.
Results
The diagnostic performance of MDCT was evaluated with CCA serving as the standard of reference. Results from the two angiographic techniques were compared. Results were presented as sensitivity, specificity, positive predictive value and negative predictive value (Table III). These measures of validity were obtained according to the following equations:
Sensitivity = (a / a + c) x 100%
Specificity = (d / b + d) x 100%
Positive predictive value = (a / a+ b) x 100%
Negative predictive value = (d / c+ d) x 100%
Whereas a=true positive cases, b=false positive cases, c=false negative cases and d=true negative cases.
Statististical analysis was done using one way ANOVA. Measures of association were calculated using Pearson's Chi square. A р value of less than 0.05 was regarded as significant. Measures of agreement were calculated using Kappa values.
The presence of stenosis was correctly identified in 46 of 56 coronary lesions (sensitivity 82%). The absence of stenosis was correctly identified in 588 of 663 segments (specificity 97%).
The positive predictive value was 71% and the negative predictive value was 98%. The corresponding results for each vessel and its assigned segments are also shown in the same table. Therefore, the accuracy of MDCT compared favorably with that of CCA in this cohort of patients.
Table IV displays the analysis of false negative results. Thirty percent of the total missed lesions were located in the branch CX artery. Another 30% of missed lesions were located in the distal LAD, diagonal, distal RCA and branch RCA segments. Finally, 30% of total missed lesions were located in the mid RCA. Three out of six lesions in this segment were missed.
Analysis of false positive results is shown in Table V. Fourteen out of the 19 overestimated lesions on MDCT were calcified (9 moderately calcified, 5 severely calcified). The remaining five overestimated lesions were noncalcified. Only 3 out of the 19 segments were judged as being of poor quality. Of interest also was the finding that 14 out the 19 overestimated lesions were reported in the left main and the proximal parts of the coronary segments.
Images were described as good, adequate and poor in 88%, 5% and 7% of cases respectively. Poor images were mainly seen in the mid RCA, distal RCA and LAD branches and were mostly attributed to motion artifacts (67%), but also equally to calcification and low contrast to noise ratio (16.5% for each factor) (see Table VI).
Discussion
Noninvasive imaging of the coronary arteries is fraught with great difficulties, namely the small dimensions of the coronary vessels, calcification of these vessels and the fact that coronary arteries are subjected to rapid motion because of cardiac contraction and respiratory movements.
The first generation sequential CT scanners produced an axial image while the table remained motionless. This scanning was both time consuming and extremely sensitive to respiratory movements and was therefore not suitable for cardiac imaging.
CT imaging of the heart and coronary arteries without motion artifact first became possible with the introduction of the electron beam computed tomography (EBCT) in 1983, which operates completely without mechanical motion, thus providing a temporal resolution of 50-100 ms (so far unsurpassed).
Initial results that were obtained with this technology were very promising though the spatial resolution and signal-to-noise ratio was found to be somewhat limited with this technique. At EBCT, a compromise has to be made between z-axis resolutions and scan coverage; so distal coronary arteries may not be included in the acquisition(10).
The total scan time was significantly reduced with the introduction of spiral CT scanners. The scan is performed while the patient is continuously moving at a pre-defined speed through the scanner. The resulting trajectory of the X- ray tube rotating around the patient can be plotted as a helix or spiral. These scanners acquire volumetric data and cross sectional images can be reconstructed later for any anatomic region. This configuration significantly reduced the total scan time(11).
Spiral or helical CT was hampered for years with gantry rotational speeds 10 times slower than EBCT, and thus was not able to avoid image blurring due to cardiac motion. Additionally, single or even dual slice imaging with the older versions of spiral CT scanners required two or more breath holds (about 40 sec) just to complete thin sectioning of the heart.
MDCT is the recent development in spiral CT. These scanners are not only equipped with multiple and thinner detector rows that leads to high spatial resolution, a prerequisite to visualize the small coronary arteries with their complex course, but also equipped with a faster X- ray tube rotation speed yielding a high temporal resolution, which is a prerequisite to visualize rapidly moving coronary arteries and allow shorter scanning time that makes possible performing the test during a single breath hold(12). Retrospective gating allows post-scan acquisition window selection and optimum gating during the diastolic phase of the cardiac cycle. This approach improves image quality and ensures the least cardiac motion artifacts.
The resolution of the MDCT continued to improve with advent of the 16 row scanners. They acquire thinner slices up to 16 images per rotation and rotate faster, with a rotational speed of about 400 to 500 ms per revolution. Well-planned clinical trials using this technology showed extremely improved results in comparison to the 4-row scanners(6,7). Results that can be achieved however depend very strongly on the group of patients that are studied and on how much CAD is prevalent among these patients. To achieve reliable results, it is mandatory to pre select the patients group.
Our purpose in this study was to report our initial experience in evaluating the role of 16-slice MDCT in non-invasive detection of presence and extent of CAD, and compare it to CCA at a major tertiary cardiac center in Jordan (QAHI) that serves the public sector.
By analyzing the results for the whole set of studied segments, it looks clear that the accuracy of MDCT compared favorably with that of CCA in this cohort of patients and is in keeping with several recently published reports using the same scanner 13-16.
Regarding the false negative results, it looks evident that out of the 21 true proximal lesions in the LAD, C and RCA vessels and the true 12 lesions in the mid LAD and C arteries, only one lesion was missed in the mid LAD segment by MDCT which was described as being of good quality and of being non calcified. So the likelihood of missing a lesion in all the proximal and mid segments except the mid RCA segment is very small.
Thirty percent of the total missed lesions in our study group were located in the branch CX artery in keeping with previous reported studies. This artery is more difficult to evaluate, probably because of its tortuous course and overlapping structures.
It easily blends with the adjacent contrast filled structures such as the great cardiac vein and the left atrium(8) None of the three lesions in this branch were correctly diagnosed raising a big question mark and leading to a low sensitivity for detecting disease of the segment. Another 30% of lesions were located in the distal LAD, Diagonal, distal RCA and branch RCA segments suggesting lower diagnostic performance of MDCT angiography in small caliber branches with distal location.
Thirty percent of total missed lesions were located in the mid RCA. Three out of six lesions in this segment were missed. This segment remains mobile during the cardiac cycle and runs perpendicular to transverse slices; consequently, this vessel is more vulnerable to arrhythmia and inaccurate triggering which results in discontinuity between the consecutive cycles(8). Therefore, the majority of missed lesions were located in distal segments and side branches in addition to mid RCA segment.
Sensitivity, specificity, positive predictive and negative predictive values would certainly be higher if we excluded these segments. Since complete visualization of all clinically important coronary segments is a prerequisite for any coronary angiographic modality to become an accepted tool for the assessment of patients with suspected CAD, the non-invasive MDCT modality clearly falls short of the diagnostic superiority of CCA for the time being.
Regarding the false positive results we had in this study, it looks that the majority of them were related to calcification (74%) and were located in the proximal segments of the studied vessels.
It is known that overestimation of calcified lesions is usually related to beam-hardening artifacts and partial volume effects resulting in blooming of the coronary arteries(14).
The calcified segments rendered images that were described as being of poor quality only in three out of 19 segments, while in the remaining overestimated segments the images were read with moderate or even great confidence. The majority of these lesions appeared as wall irregularities on CCA.
It was found that improvements in spatial resolution and dedicated post processing algorithms might diminish the problem of overestimation by calcification. Coronary calcium quantification correlates with the extent of atherosclerosis, but severely underestimates the total coronary plaque burden. In fact, the amount of calcium detected with EBCT reflects only one fifth of the measured atherosclerotic plaque burden(17).
A good correlation between calcium scoring with EBCT and MDCT scanners has been described. Most studies on calcium scoring have been performed using EBCT scanners, but nowadays this will gradually be taken over by MDCT scanners, which are widely available(18).
Applied radiation dose of MDCT still remains higher than selective coronary angiography and this is an important limitation for the technology(19,20). Dose measurements in our institution yielded effective doses of 728 mGy/cm2 versus 320 mGy/cm2 for CCA.
It is clearly not the prime time to consider MDCT as an alternative to CCA. Subtle details of small collateral vessels, small coronary branch arteries, calcific segments and regions such as mid RCA may be obscured, lost or overestimated. Furthermore, the clinical value of MDCT coronary angiography needs to be established in multi-centre studies, evaluating populations with differing prevalence and presentations of coronary atherosclerosis.
Conclusion
MDCT is quite sensitive and highly specific in the detection of coronary artery disease in our cohort of patients in sinus rhythm with stable angina. However further improvements in spatial and temporal resolution are still required to challenge diagnostic CCA.With the current introduction of new 64-detector CT scanners with faster gantry rotation and thinner collimation, we hope to get better results and therefore accelerate MDCT implementation in clinical practice.
Acknowledgments We thank our radiographer Mahmoud Al-Sholool for his excellent work and his continuous dedicated commitment to our study.
Table I: Patient characteristics in the study group
|
Total number of patients
|
50
|
|
Gender Male
Female
|
39
(78%)
11(22%)
|
|
Mean age (yrs) ± SD
|
54
±7.2
|
|
Mean Heart rate( beats/min)
± SD
|
66.2
± 10.2
|
|
Mean BMI (kg/m2) ± SD
|
26.2
± 2.9
|
|
Extent of CAD
|
|
|
Normal
|
17
(34%)
|
|
Single vessel disease
|
19(38%)
|
|
Two vessel disease
|
9
( 18%)
|
|
Three vessel disease
|
5
(10%)
|
|
Cigarette smoking
|
39(78%)
|
|
Hyperlipidemia
|
24(48%)
|
|
Hypertension
|
35(70%)
|
|
Diabetes
|
22(44%)
|
|
Family history of CAD
|
10(20%)
|
Table II. Definitions of image quality and amount of calcification
|
Image quality
|
|
|
Good
|
Allowed with great
confidence due to the absence of any artifacts (motion, noise, and
calcification).
|
|
Adequate
|
Allowed with moderate
confidence due to artifacts.
|
|
Poor
|
Allowed with very low
confidence
|
|
Amount of calcification
|
|
|
None
|
Neither plaques nor speckles
noticed.
|
|
Mild to moderate
|
Small and isolated amounts
noted.
|
|
Severe
|
High density lesions.
|
Table III: Detection of significant stenosis with 16-Row multidetector computed tomography coronary angiography
|
Coronary segments
|
N
|
TP
|
TN
|
FP
|
FN
|
Sensitivity
%
|
Specificity
%
|
PPV
%
|
NPV
%
|
Kappa
Value
|
P Value
|
|
All segments
|
663
|
46
|
588
|
19
|
10
|
82
|
97
|
71
|
98
|
0.76
|
<0.00001
|
|
LM
|
149
|
0
|
146
|
3
|
0
|
-
|
98
|
-
|
100
|
0.98
|
<0.00001
|
|
LAD
|
196
|
23
|
162
|
8
|
3
|
88
|
95
|
74
|
98
|
0.78
|
<0.00001
|
|
Proximal
|
50
|
7
|
39
|
4
|
0
|
100
|
91
|
64
|
100
|
0.70
|
<0.00001
|
|
Mild
|
48
|
7
|
37
|
3
|
1
|
88
|
93
|
70
|
97
|
0.73
|
<0.00001
|
|
Distal
|
49
|
2
|
46
|
0
|
1
|
67
|
100
|
100
|
98
|
0.80
|
<0.00001
|
|
Branch
|
49
|
7
|
40
|
1
|
1
|
88
|
98
|
88
|
98
|
0.85
|
<0.00001
|
|
CX
|
143
|
9
|
128
|
3
|
3
|
75
|
98
|
75
|
98
|
0.73
|
<0.00001
|
|
Proximal
|
50
|
1
|
46
|
2
|
1
|
50
|
96
|
33
|
98
|
0.40
|
<0.003
|
|
Mild
|
48
|
5
|
41
|
1
|
1
|
83
|
98
|
83
|
98
|
0.83
|
<0.00001
|
|
Branch
|
45
|
3
|
41
|
0
|
1
|
75
|
100
|
100
|
98
|
0.71
|
<0.00001
|
|
RCA
|
175
|
14
|
152
|
5
|
4
|
78
|
97
|
74
|
97
|
0.74
|
<0.00001
|
|
Proximal
|
50
|
5
|
40
|
5
|
0
|
100
|
89
|
50
|
100
|
0.62
|
<0.00001
|
|
Mild
|
45
|
6
|
36
|
0
|
3
|
67
|
100
|
100
|
92
|
0.75
|
<0.00001
|
|
Distal
|
42
|
2
|
39
|
0
|
1
|
67
|
100
|
100
|
98
|
0.70
|
<0.00001
|
|
Branch
|
38
|
1
|
37
|
0
|
0
|
100
|
100
|
100
|
100
|
1.00
|
<0.00001
|
N: Normal, TP: true positive, TN: true negative, FP: false positive, FN: false negative, PPV: positive predictive value,
NPV: negative predictive value, LM: left main coronary artery, LAD: left anterior descending artery,
CX: circumflex coronary artery, RCA: right coronary artery
Table IV:Analysis of false negative results
|
Segment
|
N
|
Poor
quality
|
Calcium
score of mentioned segments
|
|
0
|
1
|
2
|
|
Branch Cx
|
3
|
0/3
|
3
|
|
|
|
Mid RCA
|
3
|
1/3
|
3
|
|
|
|
LAD
Mid
Distal
Branch
|
1
1
1
|
0/3
|
1
1
|
|
1
|
|
Distal RCA
|
1
|
0/1
|
1
|
|
|
|
Total number
|
10
|
1/10
|
1
seg. calcific
|
Table V: Analysis of false positive results
|
Segment
|
N
|
Poor
quality
|
Calcium
score of mentioned segments
|
|
0
|
1
|
2
|
|
Left main
Mid
Distal
|
1
2
|
0/3
|
0
0
|
1
1
|
0
1
|
|
LAD
Proximal
Mid
Branch
|
4
3
1
|
2/8
|
1
2
0
|
1
0
1
|
2
1
0
|
|
Cx
Proximal
Mid
|
2
1
|
1/3
|
0
1
|
1
0
|
1
0
|
|
Proximal RCA
|
5
|
0/5
|
1
|
4
|
0
|
|
Total number
|
19
|
3/19
|
5
|
9
|
5
|
Table VI: Image quality, causes and distribution of poor quality images.
|
Image
quality
|
N
/ ( %)
|
Cause
of poor quality
|
N/
(%)
|
Distribution
of poor images
|
N
(%)
|
|
Good
|
584
(88%)
|
Motion
artifact
|
28
(67%)
|
Mid
RCA
|
8 ( 19%)
|
|
Adequate
|
37
( 5%)
|
Calcification
|
7 (16.5%)
|
Distal
and branch RCA
|
8 ( 19%)
|
|
Poor
|
42 (7%)
|
Low
contrast to noise ratio
|
7(16.5%)
|
Distal
LAD and Diagonal
|
7 ( 17%)
|
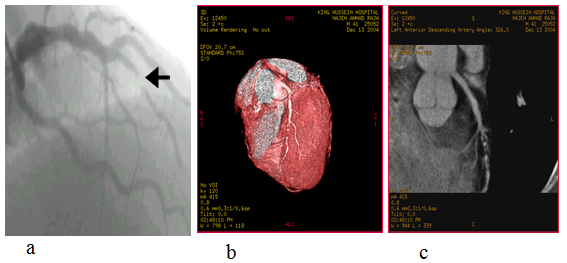 Fig. 1:
Fig. 1: Conventional coronary angiogram (a) showing subtotal post-second diagonal left anterior descending artery occlusion with late filling (Arrow). Excellent image quality of the lesion is displayed by the corresponding three -dimensional volume rendering reconstruction (b) and the maximum intensity projection images (c)