Objective: To determine the spectrum and etiology of chronic renal failure, for patients followed up in the pediatric nephrology clinic at King Hussein Medical Center, as well as to determine the prevalence and other demographic features for patients with chronic renal failure in Jordan.
Methods: A registry analysis of all children with chronic renal failure followed in the pediatric nephrology clinic at King Hussein Medical Center during the year 2004 was conducted. Chronic renal failure was defined as having glomerular filtration rate < 80 ml / min / 1.73m2. Demographic data such as sex, height, and date of birth, as well as the serum BUN, creatinine, diagnosis and the duration of chronic renal failure at the time of follow up were all recorded. Chronic renal failure was calculated from serum creatinine based on Schwartz formula. CRF was divided to 4 stages according to the Kidney Disease Outcomes Quality Initiatives guidelines, for stratification of chronic kidney disease. A total number of 117 patients, 64 (54.7%) males, and 53 (45.3%) females were included in the study. Statistical Package for Social Studies version 10 was used to analyze the data. Values are given in means ± standard deviation unless otherwise stated.
Results: The mean age was 8.6 ± 4.7 years, and the mean duration of follow up was 6.7± 2.3 years. The mean glomerular filtration rate for the whole study population at the time of recording was 28.6 ± 19.58 ml/min/1.73m2. It was shown that the prevalence of chronic renal failure among Jordanian children in the year 2004 to be 75 patients per million-child population. The most common cause of chronic renal failure was Reflux Nephropathy (30.8%) of total, followed by Neurogenic Bladder (17.9%). Reflux Nephropathy, and Obstructive Uropathy were more common in males when compared to females; where as Neurogenic Bladder and Hemolytic Uremic Syndrome were more common in females. The most common cause of chronic renal failure in patients with end stage renal disease at King Hussein Medical Center was glomerulonephritis (19.4%), followed by oxalosis (16.1%).
Conclusion: The etiology of chronic renal failure in Jordan is similar to other places with some peculiar features that need further study including the high prevalence of neurogenic bladder, and oxalosis. The importance of establishing a national and possibly regional registry system for pediatric chronic renal failure is well illustrated by this study.
Keywords: Chronic renal failure, End stage renal disease, Glomerulonephritis.
JRMS April 2008; 15(1):17-22Introduction Chronic renal failure (CRF), although rare in children when compared with adults, is considered a significant cause of morbidity and mortality in the pediatric age group(1,2) especially in developing countries where resources are limited. Early identification and management of CRF is currently the main concern of pediatric nephrologists. Recent advances in renal replacement therapy in the pediatric age group, including renal transplantation, mandates that children with CRF be identified as early as possible to prevent the associated co-morbidities, as well as to slow the progression of CRF.(1,2)
Etiology, incidence, and prevalence of CRF are not well documented in Jordan, mostly due to the absence of a National Data Registry System. In this study we define causes as well as other demographic features of Jordanian children with CRF, followed at King Hussein Medical Center (KHMC).
MethodsThis is a registry analysis of all patients with CRF followed in the pediatric nephrology clinic at KHMC during the year 2004. This center is the largest tertiary hospital in Jordan, and receives patients from all around the country through Royal Medical Services (RMS) peripheral hospitals. All patients with CRF from these hospitals are referred to KHMC, as it is the only hospital offering advanced pediatric renal medicine.
KHMC has all the diagnostic tools needed in modern renal medicine including isotope imaging, Magnetic Radiologic Imaging (MRI) as well as kidney biopsy, and offers various modes of renal replacement therapy including pediatric renal transplantation. Prevalence was calculated based on the fact that 35% of the populations of Jordan, (5.5 million), of which 50% are children less than 15 years of age are managed by hospitals related to the RMS. For accuracy patients with CRF followed in our clinic that are not covered by the RMS where excluded from the study when prevalence was calculated.
All patients with CRF, and a calculated GFR < 80 ml/min/1.73m2 were seen in the outpatient department during the year 2004 were included in the study. Children with end stage renal disease (ESRD) on dialysis were also included. Demographic characteristics such as age, gender, height, and weight as well as the diagnosis, and serum creatinine were recorded for all patients.
The stage of CRF was defined according to the calculated GFR using the Schwartz formula(3-5) based on height and serum creatinine at the time of recording for all children included. Patients were categorized into 4 groups according to Kidney Disease Outcomes Quality Initiatives (KDOQI) guidelines,(6) mild CRF (GFR 80-50ml/min/1.73m2), moderate CRF (GFR 50-30ml/min/1.73m2), severe CRF (GFR 30-15ml/min/1.73m2), and ESRD (GFR<15 ml/min/1.73m2 or patients on dialysis).
The diagnosis of glomerulonephritis was based on kidney biopsy findings. The duration of follow up was calculated from the time the patient was first seen in the pediatric nephrology clinic till the time of recording.
Data collected was analyzed using the Statistical Package for Social Studies (SPSS) version 10 for windows. Values are given in means ± standard deviation unless otherwise indicated.
ResultsA total number of 117 patients, 64 (54.7%) males, and 53 (45.3%) females were included in the study. The mean age was 8.6 ± 4.7 years, and the mean duration of follow up was 6.7± 2.3 years.
The mean GFR for the whole study population at the time of recording was 28.6±19.58 ml/min/1.73m2.
Seventy two (61.5%) patients were covered by the RMS, thus giving a prevalence of CRF among Jordanian children in the year 2004 of 75 patients per million-child population.
The most common cause of CRF in our center for the whole study population was reflux nephropathy comprising 30.8% of total, followed by neurogenic bladder constituting 17.9% of the total as shown in Table I.
Reflux nephropathy, and obstructive uropathy were more common in males; whereas neurogenic bladder and HUS were more common in females as presented in Table II and Fig. 1.
Table I. Etiology of CRF among the study group
|
Diagnosis
|
Number
|
%
|
| Congenital abnormalities |
|
80
|
68.4
|
|
-Reflux
nephropathy
|
36
|
30.8
|
| -Neurogenic bladder |
|
21
|
17.9
|
|
-NB
without neurological deficit
|
14
|
11.9
|
|
-NB with
spinal dysraphism
|
7
|
6.0
|
|
-Obstructive
uropathy
|
12
|
10.3
|
|
-Renal
dysplasia
|
11
|
9.4
|
|
Hereditary conditions
|
16
|
13.7
|
|
-Oxalosis
|
8
|
6.8
|
| -ARPKD |
|
3
|
2.6
|
| -Nephronophthesis |
|
3
|
2.6
|
|
-Cystinosis
|
1
|
0.9
|
| -Other |
|
1
|
0.9
|
|
Glomerulopathy
|
15
|
12.8
|
|
-Mesangio-capillary
|
6
|
5.1
|
|
-Henoch-schöenlein
purpura
|
3
|
2.6
|
|
-Focal
segmental glomerulosclerosis
|
2
|
1.7
|
|
-Crescentic
GN
|
2
|
1.7
|
|
-Minimal
change disease
|
1
|
0.9
|
|
-Post
strept GN
|
1
|
0.9
|
|
Hemolytic Uremic Syndrome (HUS)
|
5
|
4.3
|
|
Rhabdomyosarcoma
|
1
|
0.9
|
|
Total
|
117
|
100
|
Table II. Etiology of CRF according to gender among the study group
|
Diagnosis
|
Gender
|
Total (%)
|
|
|
Male (%)
|
Female (%)
|
|
|
Reflux nephropathy
|
24 (37.5)
|
12 (22.6)
|
36 (30.8)
|
|
Neurogeic bladder
|
9 (14.1)
|
12 (22.6)
|
21 (17.9)
|
|
Obstructive uropathy
|
11 (17.2)
|
1 (1.9)
|
12 (10.3)
|
|
Glomerulopathy
|
8 (12.5)
|
4 (7.5)
|
12 (10.3)
|
|
Renal dysplasia
|
4 (6.3)
|
7 (13.2)
|
11 (9.4)
|
|
Oxalosis
|
2 (3.1)
|
6 (11.3)
|
8 (6.8)
|
|
HUS
|
0 (0)
|
5 (9.4)
|
5 (4.3)
|
|
ARPKD
|
1 (1.6)
|
2 (3.8)
|
3 (2.6)
|
|
Nephronephthesis
|
2 (3.1)
|
1 (1.9)
|
3 (2.6)
|
|
HSP
|
0 (0)
|
3 (5.7)
|
3 (2.6)
|
|
Cystinosis
|
1 (1.6)
|
0 (0)
|
1 (0.9)
|
|
Rhabdomyosarcoma
|
1 (1.6)
|
0 (0)
|
1 (0.9)
|
|
Other
|
1 (1.6)
|
0 (0)
|
1 (0.9)
|
|
Total
|
64 (100)
|
53 (100)
|
117 (100)
|
Table III. Stage of CRF (ml/min/1.73m2) among the study group
|
|
Number
|
%
|
| Mild GFR (50 – 80) |
|
21
|
17.9
|
| Moderate (GFR 30 – 50) |
|
33
|
28.2
|
| Severe GFR (10 – 30) |
|
32
|
27.4
|
| ESRD (GFR <15) |
|
31
|
26.5
|
| Total |
|
117
|
100.0
|
RN: Reflux nephropathy, HUS: Hemolytic uremic syndrome,
GN: Glomerulonephritis ARPKD: Autosomal recessive polycystic kidney disease, HSP: Henoch Schoenlein Purpura, NB: Neurogenic bladder
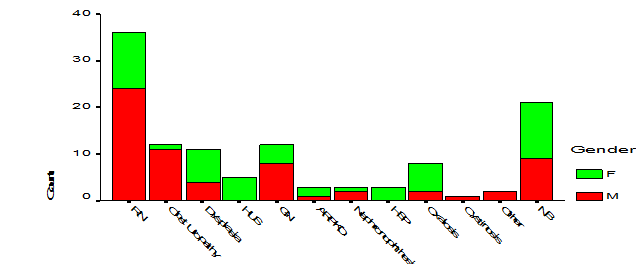 Fig. 1.
Fig. 1. Etiology of CRF according to gender
Table IV. Etiology of CRF according to severity among the study group
|
Diagnosis
|
Number (%)
|
Total number (%)
|
|
|
Mild
GFR 50 - 80
|
Moderate GFR 30 - 50
|
Severe
GFR 10 - 30
|
ESRD
GFR <15
|
|
|
Reflux nephropathy
|
7 (33)
|
12 (36)
|
13 (41)
|
4 (13)
|
36 (31)
|
|
Neurogenic bladder
|
4 (19)
|
7 (21)
|
5 (16)
|
5 (16)
|
21 (18)
|
|
Obstructive uropathy
|
3 (14)
|
4 (12)
|
4 (13)
|
1 (3.2)
|
12 (10)
|
|
Renal dysplasia
|
1 (5)
|
2 (6)
|
4 (13)
|
4 (12)
|
11 (9)
|
|
Glomerulopathy
|
2 (10)
|
3 (9)
|
1 (3)
|
6 (19)
|
12 (10)
|
|
Oxalosis
|
0(0)
|
1 (3)
|
2 (6)
|
5 (16)
|
8 (7)
|
|
HUS
|
2 (10)
|
2 (6)
|
0 (0)
|
1 (3)
|
5 (4)
|
|
HSP
|
0 (0)
|
0 (0)
|
0(0)
|
3 (10)
|
3 (3)
|
|
ARPKD
|
0 (0)
|
1 (3)
|
1 (3)
|
1 (3)
|
3 (3)
|
|
Nephronophthesis
|
2 (10)
|
0 (0)
|
1 (3)
|
0 (0)
|
3 (3)
|
|
Cystinosis
|
0(0)
|
0(0)
|
0(0)
|
1 (3)
|
1 (1)
|
|
Other
|
0(0)
|
0(0)
|
1 (3)
|
0(0)
|
1 (1)
|
|
Rhabdomyosarcoma
|
0(0)
|
1 (3)
|
0(0)
|
0(0)
|
1 (1)
|
|
Total
|
21 (100)
|
33 (100)
|
32 (100)
|
31 (100)
|
117 (100)
|
HUS: Hemolytic Uremic Syndrome, HSP: Henoch Schoenlein Purpura, ARPKD: Autosomal recessive polycystic kidney disease
The most common stage of CRF patients was stage 3 or moderate (GFR < 30 - 50 ml/min/1.73m2) CRF comprising 28.2% of total, followed by ESRD (GFR < 15 ml/min/1.73m2 or dialysis) constituting 26.5% of the total study group as presented in Table III.
Table IV shows that the most common cause of CRF in patients with ESRD was GN (19.4%), followed by oxalosis (16.1%).
DiscussionThe epidemiology of CRF in the Arab world in
general and in Jordan in particular is very scant, due to the absence of a national as well as Regional Registry System for patients with CRF. The causes as well as demographics of patients with CRF vary between countries and in different reports, which makes such a statistical analysis important aiming at early identification of patients with high risk of developing CRF, and eventually ESRD. Based on the fact that King Hussein Medical Center is the largest tertiary hospital in Jordan, we assume that the data presented in this study is an estimate of Jordanian children in general.
As in the adult population renal disease in children is more common in males than females.(3) Our results confirm the presence of male predominance regarding paediatric CRF in general in Jordan and matches well with other reports from elsewhere.
The prevalence of pediatric chronic renal failure (CRF) is not well defined and difficult to establish world wide, more so varies from one place to another. In the UK the reported prevalence in the year 1992 was 44.2 per million age-adjusted population,(7) where as in Sweden the reported prevalence in 1994 was 21 per million age-adjusted population(8,9) (defining CRF as GFR < 30 ml/min/1.73m2) .
The Italkid Project(10) reported a prevalence of CRF in Italian children of 74.7 per million child population, when patients with mild and moderate CRF were included (defining CRF as GFR < 75 ml/min/1.73m2). Compared with these figures the prevalence in our study among Jordanian children being 75 per million age adjusted population matches well with what has been reported in the Italkid study,(10) as we have defined CRF as GFR < 80 ml/min/1.73m2. Taking into consideration that all suspected children with CRF from hospitals distributed throughout Jordan, are referred to our center for follow up, we believe that this prevalence can be a fair estimate of the prevalence among Jordanian children in general.
The mean GFR at the time of registration for the whole study population (28.6±19.58 ml/min/1.73m2) is considered low. This study indicates that > 60% of patients with CRF followed up in the pediatric renal clinic have severe CRF and ESRD (GFR < 30 ml/min/1.73m2. This can be partly explained by the general setup, and scantiness of renal medicine in the peripheral hospitals related to the RMS and again raises the issue of late referrals, as well as the decreased awareness of the general pediatrician regarding the importance of early identification and proper follow up of children with CRF.
The commonest cause of CRF in our study being reflux nephropathy (30.8%), matches well with other reports from developed as well as developing countries.(8-11)
Congenital abnormalities in general remain the commonest cause of CRF in children.(1-3,8,9,12) In our study, congenital abnormalities comprised more than 68% of patients followed by hereditary conditions comprising 13.7% of children with CRF and this matches well with data from the Italkid study(10) and elsewhere.
It is well known that isolated vesico-ureteric reflux (VUR) in the general population is more common in females with a female to male ratio of 4:1.(15) Our data indicates that VUR causing CRF is more common in males with a male to female ratio of 2:1, which matches well with what has been reported in the Italkid study,(10) and again raises the issue that children with VUR causing CRF do not come from the same population of children having isolated VUR and questions the use of reflux nephropathy as a term to indicate absolute cause and effect relationship.
Acquired glomerupathies comprised only 12.8% of the total patients with CRF. This figure matches well with reports coming from the United Kingdom and Sweden, where acquired glomerulonephritis was the cause of CRF in 10.3%(7) and 14.4%(8) of total respectively. In the United States, data from the North American Pediatric Renal Transplant Cooperative Study Group (NAPRTCS),(9) indicate that glomerulonephritis was the cause of CRF in 22% of patients. The increased incidence in the United States is mainly attributed to a high incidence of focal segmental glomerulosclerosis (FSGS) in African Americans when compared with other parts of the world.
Another point of importance is that in our study acquired glomerulonephritis was the most common cause of CRF in patients reaching ESRD, comprising 19.4% of patients with ESRD. This indicates what has been reported earlier regarding the rapid progression of acquired glomerulopathies when compared with congenital and hereditary conditions.(14) A high percentage of primary hyperoxaluria is noted as well in our patients especially those reaching ESRD, and was the second most common cause after acquired glomerulopathies in these patients. Although these figures are very high when compared to figures coming from the developed world,(7-10,12) it matches well with other reports coming from the region(11) and may be explained by the high rate of consanguinity in Jordan.
The incidence of neurogenic bladder in our patients (17.9%) is very high when compared with reports from other places, furthermore only one third (33.3%) of these patients had neurological abnormalities and the rest were classified as having nonneurogenic bladders (Hinnman Syndrome). Although these figures are striking, and are not readily explainable, it is important to mention that such high figures were reported previously in Jordan.(13) This phenomenon should be further studied and evaluated in Jordan.
A plausible explanation may well be the decreased awareness of physicians regarding the importance of early identification and referral of patients with a high risk of having a neurogenic bladder, as we have noticed that a high percentage of these patients are only referred after they start having renal impairment.
ConclusionThe characteristics of chronic renal failure in Jordan, although similar to what has been reported elsewhere; has some peculiar features. The high incidence of neurogenic bladder and hyperoxaluria as a cause of chronic kidney disease mandates further studies.
This study also shows that late referrals is currently a problem in Jordan and illustrates the importance of educating primary care physicians regarding the importance of early referral and proper follow up of patients with mild chronic kidney disease, aiming at slowing progression, and avoiding associated co-morbidities.
The importance of establishing a national registry system is also well illustrated in this study.
References
1. Harmon WE. Overview of chronic renal failure. In: Barratt TM, Avner ED, Harmon WE, Eds. Pediatric nephrology, 4th Edn, Lippincott Williams and Wilkins. 1999; 1151 - 1154
2.Susan PA. Rigden. The management of chronic and end stage renal failure in children. In: Webb N, Postlethwaite R Eds. Clinical pediatric nephrology, 3rd Edn, Oxford University Press. 2003; 426-445
3. Nissenson AR, Pererra BJ, Collins AJ, Steinberg EP. Relevance and characteristics of individuals with chronic kidney disease in a large health maintenance organization. Am J Kidney Dis 2001; 37(6):1177-1183.
4. SchwartzGJ, Haycock GB, Edelman CM, Spitzer A. A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 1976; 58: 259-263.
5. Counahan R, Chantler C, Ghazali S, et al. Estimation of glomerular filtration rate from plasma creatinine in children. Arch Dis Child 1976; 51: 875-78l.
6.K/DOQI. Clinical practice guidelines for chronic kidney disease: Evaluation classification and stratification. Am J Kidney Dis 2002; 39(2): S46-S75.
7. Report of a Working Party of the British Association for Pediatric Nephrology 1995: The provision of services in the United Kingdom for children and adolescents with renal disease. London: British Pediatric Association.
8. Esbjorner E, Berg U, Hansson S. Epidemiology of chronic renal failure in children: A report from Sweden 1986-1994. Pediatr Nephrol 1997; 11: 438-442.
9.Seikaly M, Ho PL, Emmett L, et al. Chronic renal insufficiency in children: the 2001 Annual Report of the NAPRTCS. Pediatr Nephrol 2003; 18(8): 796-804.
10. Ardissino G, Daccò V, Testa S, et al. Epidemiology of chronic renal failure in children: Data From the Ital Kid Project Pediatrics 2003; 111: 382-387.
11. Madani K, Otoukesh H, Rastegar A, Van Why S. Chronic renal failure in Iranian children. Pediatr Nephrol 2001; 16(2):140-144.
12.Peco-Antic A, Bogdanovic R, Godubovic E, Djapic M. Chronic renal failure in children in Yugoslavia. Srp Arh Celok Lek 2003;131(1-2):5-9.
13.Hamed RM. The spectrum of chronic renal failure among Jordanian children. J Nephrol 2002; 15(2):130-135.
14. Deleau J, Andre JL, Briancon S, Musse JP. Chronic renal failure in children: An epidemiological survey in Lorraine (France) 1975-1990. Pediatr Nephrol 1994; 8(4): 472-476.
15.Macedo CS, Bastos HD, Riyuzo MC. Renal scars in children with primary vesicoureteral reflux. Journal de Pediatria 2003; 79(4): 12-15