ABSTRACT
Objective: Radiology
plays a crucial role in diagnosis, work-up and staging of osteosarcoma. The
main aim of the study is to review, analyze and characterize the imaging
findings of a large series of histologically proven osteosarcomas focusing on
the nonconventional subtypes.
Methods: We retrospectively reviewed the imaging findings of 250 cases with histologically proven primary osteosarcoma. The study was conducted at King Hussein Medical Center and King Hussein Cancer Center, Amman-Jordan during the period 2003-2012. Approval by the ethical committee and institutional review board was taken from both institutions before starting the study. Patient demographic data was recorded. Images from plain radiographs (n =238 ), angiograms (n =28), bone isotope scans (n =56), computed tomography scans (n =99), computed tomography angiograms (n=27 ) and magnetic resonance imaging (n =189 ) were evaluated for the origin site, location, tumor size, matrix pattern, extrinsic and intrinsic characteristics and the soft tissue component of the tumor. The sample included 162 males (65%) and 88 females (35%), with an age range of 12-48 years (mean age of 23.5 years). Simple descriptive statistical methods (frequency, mean and percentage) were used to describe the study variables.
Results: The most common histological diagnoses were conventional (n=193), telangiectatic (n=14), small cell (n=3), low grade central (n=3), high grade surface (n=2), parosteal (n=4), and periosteal (n=5) and non specific (n= 26). The most frequent origin site in the long bones is the metaphysis (80%) followed by diaphysis (9% ), and less frequently the epiphysis (2%), 10% were found in the spine and flat bones. The commonest lesion location was distal femur (25%), proximal femur (18%), proximal humerus (17%), proximal tibia (15%), spine and flat bones (16%), other places (9%). The tumor size ranged from 2-21cm. The majority of cases (78%) demonstrated osteoid matrix abnormal mineralization, 32 of them showed obvious and marked mineralization, three cases with marked mineralization were noted in the spine, one of them gave an ivory vertebra appearance. A purely lytic pattern was seen in 48%. Soft-tissue components were seen in 58% of cases.
Conclusion: This study provides a good relation between the radiological imaging and histological subtypes of osteosarcoma in a relatively large series of osteosarcoma and highlights our experience at King Hussein Medical and Cancer Centers.
Key words: Osteosarcoma, Radiological Evaluation
JRMS September 2013; 20(3): 13-20 / DOI: 10.12816/0001035
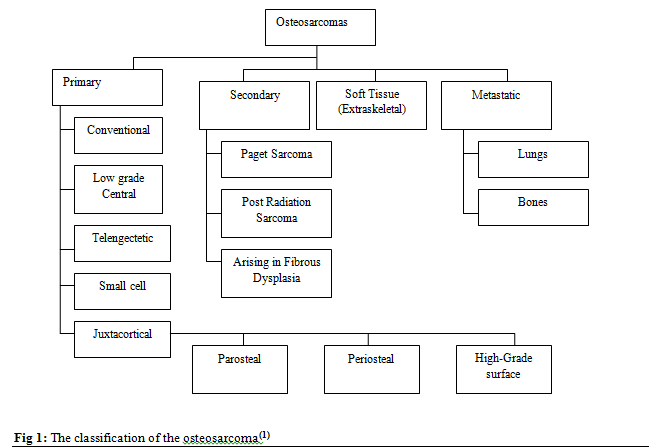
Fig 1: The classification of the osteosarcoma(1)
Introduction
Osteosarcoma (OS) is a malignant tumor of the bone. It is arising from primitive mesenchymal bone-forming cells. It is characterized by osteoid matrix production. It may also produce some variable amounts of cartilage matrix and fibrous tissue. It usually arises as a solitary tumor in the fastest growing part of the long bones.(1) It was firstly described in 1805, by a French surgeon Alexis Boyer (personal surgeon to Napoleon) who used the term osteosarcoma as a distinct entity different from other bone lesions, such as osteochondromas (exostoses).(2) The World Health Organization classification of OS includes eight categories: the commonest and the classical form is conventional OS, other less common subtypes include telangiectatic, small cell, low-grade central, parosteal, periosteal, high-grade surface and secondary, Fig. 1.(1)
Not all osteosarcomas arise as a solitary lesion, as multiple sites may become apparent within a period of about 6 months (synchronous osteosarcoma), or multiple sites may be noted over a period longer than 6 months (metachronous osteosarcoma).(3) Although OS accounts for less than 1% of all cancers, but it is considered to be the commonest primary bone tumor in children and adolescents.(1,4,5) The nonconventional (subtypes) OS have distinct radiological appearances that may mimic different benign and malignant entities. The prognosis, outcome, and the mode of treatment differ from one subtype to another, this make it essential to give correct diagnosis which requires recognition of characteristic imaging findings. In this study, a review and summary of the imaging variations of OS was performed. An attempt to offer a schema for it OS subs classification, characteristics appearance and differential diagnostic considerations. There was more concentration on nonconventional subtypes and other malignant and benign entities that may resemble them radiologically.
Methods
A retrospective thorough revision for the imaging findings of 250 cases with histologically proven primary OS during the period 2003-2012 was done by a musculoskeletal radiologist with 17 years of experience. The review included plain X-ray, CT scan, CT angiogram, ultrasound reports, bone isotope scan, conventional angiogram, interventional procedures including biopsies and MRI. The study was conducted at King Hussein Medical Center linked with the Royal Center of Rehabilitation and Orthopedics and King Hussein Cancer Center, Amman-Jordan. An approval by the ethical committee and institutional review board was taken from both institutions before starting the study. Informed consent was not required. Patient demographic data was recorded. Images from plain X-ray (n = 238), angiogram (n =28), bone isotope scan (n =56), CT scan (n =99), CT angiogram (n= 27) and magnetic resonance imaging (n =189) were evaluated. The evaluation was aimed toward the origin site of the tumor (metaphysis, diaphysis, or epiphysis), location of the bulk of the tumor (anterior, posterior, medial, lateral or combination of them), tumor size (measured in two perpendicular diameters for the largest and smallest measures), matrix pattern (purely lytic, sclerotic or mixed), extrinsic and intrinsic characteristics, periosteal reaction (either nonaggressive with solid cortical thickening or aggressive showing a Codman triangle or having an irregular appearance) and finally the soft tissue component of the tumor (the compartments which are involved and the involvement of the adjacent neurovascular bundle).(6) The sample included 162 males (65%) and 88 females (35%), with an age range of 12-48 years (mean age of 23.5 years). Bone scintigrams were evaluated for the presence and the degree of tracer uptake. Angiograms were evaluated for the presence and degree of tumor blush and the relation of the tumor with the adjacent vessels.
CT scan images were evaluated for the presence of soft-tissue masses, cortical thickening, cortical irregularity and periosteal reaction. MR images were evaluated mostly for the associated soft tissue component including the relation to the adjacent neurovascular bundle, compartments involved and mineralization of the soft tissue component. MRI images were also evaluated for the degree of the medullary invasion and edema.
The degree and pattern of enhancement was also evaluated in the post contrast study.
Simple descriptive statistical methods (frequency, mean and percentage) were used to describe the study variables.
Results
The most common histological diagnoses were conventional 77.2% (n=193), telangiectatic 5.6% (n=14), small cell 1.2% (n=3), low grade central 1.2% (n=3), high grade surface 0.8% (n=2), parosteal 1.6% (n=4), periosteal 2% (n=5) and non specific 10.4% (n=26). The most frequent origin site in the long bones is the metaphysis (80%) followed by diaphysis (9%) and less frequently the epiphysis( 2%), 10% were found in the flat bones. The commonest lesion location was distal femur (25%), proximal femur (18%), proximal humerus (17%), proximal tibia (15%), spine and flat bones (16%), other places (9%). The lesions most frequently occurred anteromedially in the long bones. The tumor size ranged from (1.3 X 2.4cms to 8.8 X 22.1 cms). The majority of cases 78% demonstrated abnormal osteoid matrix mineralization, 32 of them showed obvious and marked mineralization, three cases with marked mineralization were noted in the spine, one of them was giving an ivory vertebra appearance.
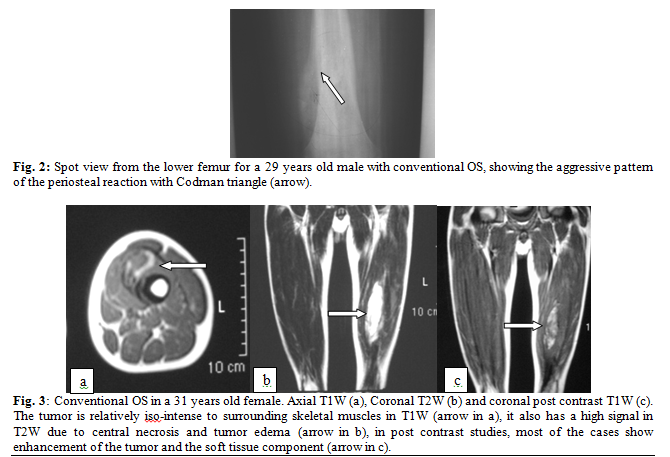
Periosteal reaction was common and noted in 69% of cases. It appeared in an aggressive form with Codman triangle in 38% of cases Fig. 2. Perpendicular periosteal reaction to the long bone shaft going toward the soft tissue component was noted in 19% of cases.
Soft-tissue components were seen in 58% of cases. Non enhanced MR imaging showed the soft-tissue component to have a similar intensity to that of surrounding skeletal muscle on T1-W images. On the other hand it appeared on T2W images to be predominantly of heterogeneous high signal intensity. MRI post intravenous gadolinium injection showed mild to moderate degree of enhancement in 58%, and a marked degree of enhancement in 33%, and no significant enhancement in only 9% Fig. 3.
In cases where the histological grade of the tumor was available, 40% were grade I, 24% were grade II, and 36% were grade III.
Discussion
Osteosarcoma is a heterogeneous group of malignant spindle cell tumors that have the ability for production of immature bone (osteoid). The degree of malignancy, and thus the tendency to metastasize, is determined by the histological grade(7) as prognosis of OS continues to improve particularly with the era of limb salvage surgery, new challenges for both radiologist and orthopedic surgeons continue to arise. This discussion will highlight the imaging features of OS with more focus on various subtypes. It is essential to note that this discussion is - by no means - intended to be comprehensive; rather it is an evaluation of our experience at King Hussein Medical and Cancer Centers, Amman-Jordan.
The majority of OS are of an unknown etiology (idiopathic or primary), the minority arises from a preexisting condition and so they are labeled as secondary OS.
OS can be graded histopathologically according to Broder’s system from grade one to four; on the other hand the OS subtypes are classified into eight types.
Conventional OS:
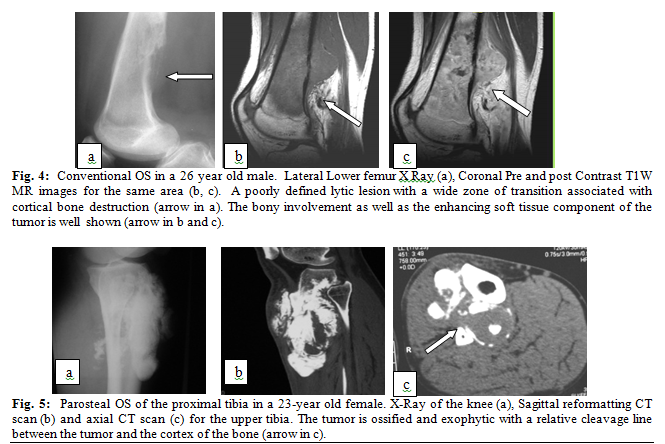
The commonest form of OS, the characteristic radiological appearance includes medullary and cortical bone destruction, malignant looking periosteal reaction and soft tissue component (Fig. 4).
The main concern of this article is on the OS subtypes, so conventional OS will not be discussed in more details.
Parosteal OS:
It is the commonest subtype of juxtacortical OS, usually arising from outer fibrous layer of the periosteum and involving the metaphyses of long bones, in particular the posterior aspect of the distal femur. It carries better prognosis than conventional OS, it is usually low grade, exhibiting minimal fibroblastic stromal atypia. The five year survival rate is 89% comparing to 57% for conventional OS.(1,8) The classical appearance at radiography is an oval or spherical mass attached to the surface of the cortex, it has a central dense ossification with a relatively clear cleavage line between the tumor and normal cortex. Thickening of the cortex with relative lack of aggressive periosteal reaction is often
apparent. CT and MRI are often needed to access the cortical penetration and medullary invasion Fig. 5. Differential diagnosis would include osteochondroma, myositis ossificans, paraosteal osteoma, periosteal chondroma, periosteal chondrosarcoma, and other subtypes of juxtacortical OS.(2,3,5)
Periosteal Osteosarcoma
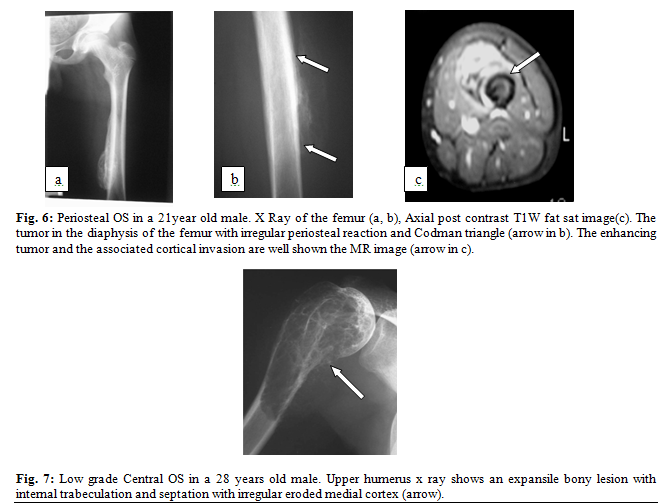
Periosteal OS arises from the innermost layer of the periosteum and considered the second most common type of juxtacortical OS, it accounts for about 1-2 % of all OS , it grows on the surface of the bone and typically affecting the diaphysis of long bones preferably the tibia.(1,9) The prognosis of periosteal OS is much better than the conventional one (83% 5-year survival rate) but still worse than parosteal OS.(10) The classical radiological appearance is an inhomogeneous tumor matrix with speculation, calcification and low attenuation uncalcified matrix. The tumor exhibits periosteal reaction and extending into the soft tissue with relative sparing of the medullary cavity and endosteal surface Fig. 6. Differential diagnosis include other types of juxtacortical OS, periosteal chondroid tumors and myositis ossificans. Periosteal chondroid tumors are juxtacortical soft-tissue tumors that are having a rather well-defined outline occuring at metaphysis. On the other hand periosteal OS is a broad-based soft-tissue mass occuring at diaphysis, and produces a cortical erosion and periosteal reaction perpendicular to the cortex.(1,6)
Low-Grade Central Osteosarcoma
This rare entity of OS was recently been recognize and described. It is arising from the medullary canal of the long bones. Low grade central osteosarcoma usually have a relatively good prognosis with a 5-year survival rate of 90% , however, it has the potential to reccur if the surgical safety margin is not adequate.(11) The radiological appearance is that of an expansile lytic lesion with internal trabeculation. It may have features of conventional OS but with less aggressive nature and slower growing rate, Fig. 7. The extension of tumor cells between mature bone trabeculae is an important point in differentiating it from benign lesions like fibrous dysplasia, nonossifying fibroma, and desmoplastic fibroma.(1,7,8,11)
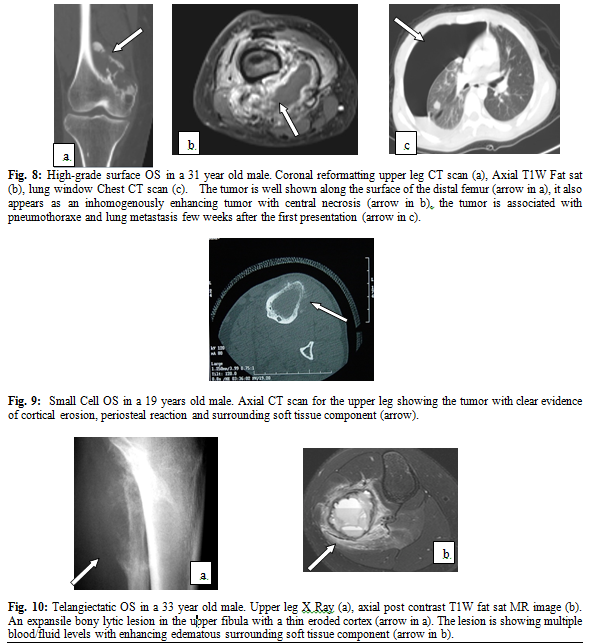
High-Grade Surface Osteosarcoma
It is the least common type of juxtacortical OS. The tumor is usually large and may reach up to 25cms. The radiological appearance includes malignant looking periosteal reaction, irregular shape dense ossification, cortical thickening and erosion. Differential diagnosis include parosteal OS, periosteal OS, and conventional OS(1,8,12) (Fig. 8).
Small Cell Osteosarcoma
The tumor appears as a permiative radiolucent lesion with a relatively large soft tissue component. Differential diagnosis includes Ewing sarcoma, primitive neuroectodermal tumor, lymphoma, and conventional OS. It is difficult (histologically and radiologicaly) to differentiate small cell OS from Ewing sarcoma. If dystrophic calcifications is seen, then small cell OS is favorable as calcifications rarely occur in Ewing sarcoma(1,5,8) ( Fig. 9).
Telangiectatic Osteosarcoma
It is the most aggressive type of OS. It is characterized by high degree of vascularity with large blood filled cystic spaces with necrosis. When the new adjuvant chemotherapy was implemented, the prognosis for telangiectatic OS has significantly improved. The five year survival rate has increased from 17% to 57%.(1) The classical radiological appearance is an expansile geographic bony lesion with cortical destruction. Telangiectatic OS has a characteristic MRI appearance with blood containing lesion that is exhibiting a bright signal on T1W images and variable signal intensity on T2W images. The fluid levels are quit common and differentiate telangiectatic OS from other OS subtypes.(3,8)
Differential diagnoses of telangiectatic OS is narrow but due to fluid levels, aneurysmal bone cyst (ABC) and giant cell tumor of bone have to be considered particularly the former one.
Distinguishing ABC from telangiectatic OS can be a real challenge due to great radiology and histopathology similarities between the two entities. Reviewed many articles regarding this issue, we concluded that the 3 most important features that favor telangiectatic OS than ABC are : the presence of thick solid nodular tissue surrounding the cystic spaces, the presence of matrix mineralization in the lesion, and the presence of cortical destruction with associated soft-tissue component,(1,3,8,13,14) Fig. 10. This study has some limitations. First, although 250 cases are not a small number but the need to include more cases to increase the sample size is mandatory. No inter-observer variation is included; since all the radiological observations were analyzed by one radiologist (the author) as only one musculoskeletal radiologist currently works in our institute.
Conclusion
This study provides a good correlation between the radiological imaging and histological subtypes of osteosarcoma in a relatively large series of OS cases. It also highlights our experience at King Hussein Medical and Cancer Centers. Further studies are needed to include more cases of OS to this study for better assessment.
References
1.Yarmish G, Klein MJ, Landa J, et al. Imaging characteristics of primary osreosarcoma: Nonconventional subtypes. Radio Graphics 2010; 30: 1653-1672.
2.Peltier LF. Tumors of bone and soft tissues. Orthopedics:A history and iconography. San Francisco, Calif: Norman Publishing; 1993: 264-91.
3.Klein MJ, Siegal GP. Osteosarcoma. anatomic and histologic Variants. American Journal of Clinical Pathology 2006, 125, 555-581.
4.Mirabello L, Troisi RJ, Savage SA. A comprehensive candidate gene approach identifies genetic variation associated with osteosarcoma. Cancer 2011; 11:209–218.
5.Murphey MD, Robbin MR, McRae GA, et al. The many faces of osteosarcoma. Radio Graphics 1997; 17(5):1205–1231.
6.Murphey MD, Jelinek JS, Temple HT, et al. Imaging of periosteal osteosarcoma: radiologic-pathologic comparison. Radiology 2004; 233: 129-138. Damron TA,
7.Buecker PJ, Gebhardt M, Weber K. Osteosarcoma. Electronic sarcoma update newsletter. February 2005; Vol. 2, chapter 1.
8.Greenspan A. Orthopedic Imaging. A practical approach. 5th edition, 2004.
9.Damron TA, Ward WG, Stewart A. Osteosarcoma, chondrosarcoma, and Ewing's sarcoma: National Cancer Data Base report. Clin Orthop Relat Res 2007; 459: 40-47.
10.Murphey MD, Choi JJ, Kransdorf MJ, et al. Imaging of osteochondroma: variants and complications with radiologic-pathologic correlation. Radio Graphics 2000; 20(5): 107-143.
11.Andresen KJ, Sundaram M, Unni KK, Sim FH. Imaging features of low-grade central osteosarcoma of the long bones and pelvis. Skeletal Radiol 2004; 33(7):373-379.
12.Staals EL, Bacchini P, Bertoni F. High-grade surface osteosarcoma: a review of 25 cases from the Rizzoli Institute. Cancer 2008; 112(7):1592–1599.
13.Murphey MD, Jaovisidha S, Temple HT, et al. Telangiectatic osteosarcoma: radiologic-pathologic comparison. Radiology 2003; 229(2):545–553.
14.Discepola F, Thomas I, Powell, et al. Telangiectatic osteosarcoma: radiologic and pathologic findings. Radio Graphics 2009; 29: 380-383.