ABSTRACT
Objective: To present our experience in the first 100 live liver-donors done at King Hussein Medical Center with emphasis on donor postoperative complications and possible risk factors predisposing to complications.
Methods: Over a period of 11 years 100 live-liver donors underwent surgery. Demographic, clinical and perioperative data of these donors were collected. Postoperative complications were registered and classified according to the Clavien-Dindo classification. Statistical analysis was used to identify potential patients’ or grafts’ factors associated with complications.
Results: The mean age of donors was 30.71±7.17 and mean body mass index was 24.50± 2.56. Three procedures were abandoned after laparotomy. 71 underwent right hepatectomy, 12 right hepatectomy with inclusion of middle hepatic vein, 11 left hepatectomy and 3 left lateral sectorectomy. The overall complication rate was 36% with most of these being minor grade I and II (26%) complications. 9 patients developed grade III complications while one patient had grade IVa. The mortality rate was zero. Older age and higher body mass index were identified as potential risk factors for complications. Gender, graft type, estimated future liver remnant, inclusion of middle hepatic vein and preoperative biochemical profile were not found in this study to correlate with occurrence of complication.
Conclusion: Strict donor selection and meticulous surgical procedure remain the only modifiable factors in donor hepatectomy. Continuous transparent clinical audit is mandatory to identify potentially preventable adverse outcomes.
Key words: Complications, Donor hepatectomy, Liver transplantation
JRMS SEP 2016;23(3):20-27/ DOI: 10.12816/0029069
Introduction
Liver transplantation has established its role as the definitive therapy of end-stage liver disease (ESLD).Due to shortage of cadaveric organ donation, the use of living-donor liver transplantation (LDLT) started in the 1989 in pediatric patients followed shortly by its application to adult population(1). The ethical dilemma of exposing healthy volunteer to major surgery remained an obstacle (2-3) and has led to evolution of the concept of “group risk-benefit ratio”. This has been emphasized in Vancouver Forum on the Care of the Live Organ Donor (4)which states that “Live liver donation should only be performed if the risk to the donor is justified by the expectation of an acceptable outcome in the recipient”. Thus donor safety is the crux in living liver-donor transplantation programs. In a search for perfection, investigators are trying to identify potentially modifiable risk factors associated with complications in these volunteers rather than patients.
With the scarcity of deceased donor liver transplantation (DDLT) in Jordan, LDLT remains the only viable option for patients with ESLD. The first liver transplantation in Jordan has been performed in June 2004 at King Hussein Medical Center (KHMC) in corporation with a Turkish team. Since then and till December 2015, 97 living liver donors’ hepatectomy have been performed along with 5 DDLT.
Herein we will describe our experience with emphasis on donor complications. We will also identify potential donor or graft factors associated with the development of complications.
Methods
Our program of liver transplantation has started in June 2004. To explore the possibility of liver transplantation at our center, a Turkish team has been invited to perform the procedure at King Hussein hospital. This was followed by defining requirement and prerequisites to proceed. Trainee surgeons, gastroenterologists, anesthetists, pathologists, radiologists as well as staff nurses have attended short- and long training courses in Turkey, United Kingdom and Germany. In July 2009, the first LDLT was performed by our Jordanian team without assistance.
One hundred donors underwent surgery in the period from June 2004 until December 2015for 99 patients with ESLD (one recipient required re-transplantation for hepatic artery thrombosis).
Our preoperative donor evaluation protocol is strict and standardized. Donors can quit donation at any point during workup. This multistep protocol begins by interviewing the donor. Age and comorbidities are assessed by general health questionnaire. Detailed description of the preoperative preparation protocol, surgical procedure, donor’s and recipient’s risks and recipient’s benefits are provided.
After donor willingness and relation to the recipient are assured complete blood count and ABO-typing, liver and kidney function tests, liver enzymes, coagulation lab tests, virology studies and immunologic tests are requested. Chest X-ray, liver ultrasonography(US) and electrocardiography are also done at this point. If the donor is fit for donation, based on the aforementioned studies, liver contrast-enhanced computed tomography (CECT) scan and magnetic resonance cholangiopancreatography (MRCP) are requested for assessment of anatomy of the donor’s liver and biliary tree. Liver biopsy is done selectively (i.e. estimated steatosis>10% by US or CECT-scan, body mass index (BMI)>30, positivity for hepatitis B core antibody (HBcAb), donors who are first-degree relatives of recipients with autoimmune hepatitis). Psychiatric and psychological assessments are requested and any further consultations as indicated including cardiac, pulmonary or renal consultations are obtained at this point. An informed consent is subsequently obtained from the donor.
Demographic, clinical, operative and perioperative data of theses donors were prospectively collected for analysis. All postoperative complications were registered. The most severe complication in a particular donor was graded using the Clavien-Dindo Classification of Surgical Complications(5-6)to allow statistical analysis and comparison of our results with data published in the literature. Follow up ranged from 2 months and up to 6 years after donation with an average of 1 year. Recipient death was the most common cause of dropping out follow up.
Statistical analysis was done using IBM Statistical Package for the Social Sciences software (SPSS Statistics 21). Factors including age, gender, BMI, type of hepatectomy, estimated future liver remnant (FLR), preoperative liver enzymes and total bilirubin were analyzed trying to identify potential risk factors of complications. Chi-square and one-way analysis of variance (ANOVA) tests were utilized when appropriate. A p-value less than 0.05 was considered statistically significant. Approval by our institution ethical committee was obtained for publication.
Results
Our first 100 donors were included over the study period of 11 years. 71 donors were males and the mean age was 30.71±7.17 years with a range of 19-52 years. The BMI ranged from 19.1-30.4 with a mean of 24.50± 2.56. Forty-four were first-degree relatives of the recipients with the remaining being second or third degree relatives or wife of recipients as shown in Table I.
Table I: Donor and graft characteristics.
|
Variable
|
|
|
Gender
|
71 males
29 Females
|
|
Age
(mean± SD)
|
30.71±7.17 years
|
|
BMI
(mean± SD)
|
24.50± 2.56 Kg/m²
|
|
Type
of graft (Hepatectomy)
|
Right
|
71
|
|
Right with MHV
|
12
|
|
Left
|
11
|
|
Left lateral
|
3
|
|
Abandoned
|
3
|
|
Graft
weight (mean± SD)& range
|
837.7±189.3 gm (Range 309-1140 gm)
|
|
%
of Future liver remnant (mean± SD)& range
|
42.15±11.1 (Range 24.30-76.70)
|
|
Graft-recipient
weight ratio (GRWR) & range
|
1.275±1.34 (Range 0.85-3.15)
|
|
Relationship
|
Siblings (2nd degree)
|
34
|
|
Offspring to parents (1st degree)
|
28
|
|
Parents to offspring(1st
degree)
|
16
|
|
Uncle, aunt, nephew, niece and cousins
(second & third degree)
|
14
|
|
Wife to husband
|
6
|
|
Others (emotional relative)
|
2
|
Three procedures were abandoned due to recipient death in one case (after transection of the donor liver but before division of biliary duct and vessels) and abnormalities in the donor liver in 2 cases (liver granuloma and high-grade liver fibrosis).
Of the remaining 97 donors, 71 underwent right hepatectomy, 12 right hepatectomy with inclusion of middle hepatic vein (MHV), 11 left hepatectomy and 3 left lateral sectorectomy. The mean FLR was 42.15±11.1% (Range 24.30-76.70) while the mean graft-recipient weight ratio (GRWR) was 1.275±1.34 (ranged f0.85- 3.15). Donor and graft characteristics are summarized in Table I
An overall complication rate of 36% has been reported. Most of these were minor grade I and II (26%) complications. The mortality rate was zero (Table II). Of notice, caval clamp failure necessitating allogenic blood transfusion occurred in 6 donors and it was completely preventable. As such, we have started using a vascular stapling device on the inferior vena cave before transecting the right hepatic vein. One donor developed early postoperative respiratory failure necessitating re-intubation and mechanical ventilation (grade IVa) for 24 hours but fortunately he recovered completely thereafter. This has been attributed to incomplete emergence from anesthesia.
Since we have only one grade IVa complications this was added to grade III complications as one group (Major complications requiring invasive interventions) for statistical analysis.
Table II: Complications as Classified by Clavien-Dindo Classification system
|
Clavien-Dindo Grade (total)
|
Complication
|
Number (%)
|
|
Grade
I (18)
|
Pleural Effusion
Atelectasis
Minor Bile leak
Vomiting
Prolonged Ileus
Prolonged Cholestasis
Subhepatic collection (Seroperitoneum)
|
6
4
3
2
1
1
1
|
|
Grade
II (8)
|
Caval Clamp failure necessitating
Allogenic blood transfusion
Pneumonia
|
6
2
|
|
Grade
IIIa (5)
|
Bile leak-ERCP
Biliary Stricture, Endoscopic
Dilatation
Prolonged cholestasis ERCP & Bx
|
3
1
1
|
|
Grade
IIIb (4)
|
Incisional Hernia
Biliary Stricture, Hepaticojejunostomy
Intraabdominal bleeding
|
2
1
1
|
|
Grade
IVa (1)
|
Respiratory failure (Re-Intubation)
|
1
|
|
Grade
IVb (0)
|
|
0
|
|
Grade
V (0)
|
|
0
|
|
Total
|
|
36
|
The initial 42 cases were done with the Turkish team from the start of our program till July 2009. Thereafter, 58 cases were done by us (Table III). Comparing the two eras, there was no statistically significant difference in incidence or severity of complications (p-value 0.895).
Table III: Comparison of two eras *
|
|
No complications
|
I
|
II
|
III & IV
|
Total
|
|
With
Turkish team
|
26
|
9
|
3
|
4
|
42
|
|
After
Turkish team
|
38
|
9
|
5
|
6
|
58
|
*p-value calculated by Chi-square test 0.895
By using ANOVA, higher mean age and BMI were associated with occurrence of complications. Donors who developed complications had a significantly higher mean age than those who did not. On subset analysis this was validated for major type III & IV complications but not for minor Type I and II complications (Figure1). A higher BMI was found to be a risk factor for all types of complications (Figure2).
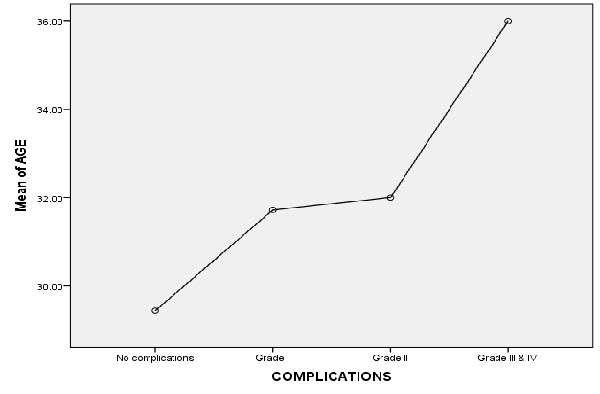
Fig.1: Mean age versus grade of complications (over all p value 0.042).
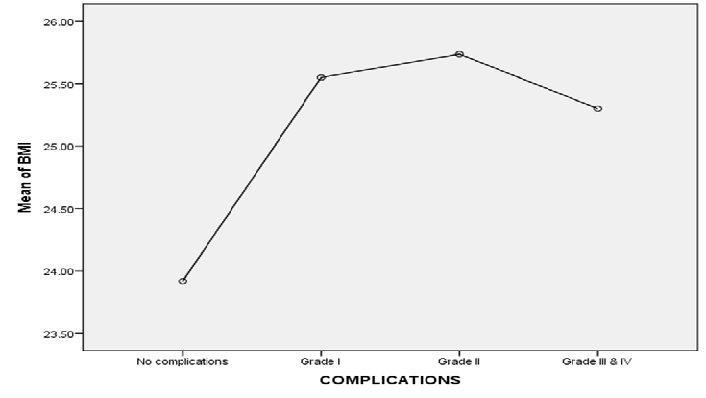
Fig.2: Mean BMI versus grade of complications (over all p value 0.024).
There was no statistically significant effect of gender, type of hepatectomy performed and estimated FLR on occurrence of complications. Since the FLR is rarely a problem in donors undergoing left hepatectomy and left lateral sectorectomy, we have re-analyzed data of donors who underwent right hepatectomy with or without inclusion of MHV. We also analyzed the impact of MHV harvesting on development of complications. Neither FLR in right hepatectomy nor inclusion of the MHV was found to significantly associated with occurrence of complications (Table III-VI).
Table IV: Donor and graft characteristics analysis.
|
Criterion / Grade
|
No
|
Grade I
|
Grade II
|
Grade III&IV
|
P value
|
|
Age
(mean± SD)
|
29.44±6.64
|
31.72±6.82
|
32.0±6.14
|
36.0±9.67
|
Overall 0.042*
Grade I 0.773
Grade II 0.906
Grade III&IV 0.040*
|
|
BMI
(mean± SD)
|
23.92±2.42
|
25.55±2.26
|
25.74±3.26
|
25.3±2.54
|
0.024*
|
|
Gender
(% males)
|
65.63
|
77.78
|
87.5
|
80
|
0.398
|
|
%
FLR (mean± SD)-Overall
|
44.63±15.02
|
40.19±15.88
|
38.58±5.12
|
45.34±16.62
|
0.516
|
|
%
FLR (mean± SD) in Right hepatectomy
|
38.43±5.23
|
36.67±5.57
|
38.58±5.11
|
35.14±2.16
|
0.307
|
*P<0.05 significant
None of preoperative biochemical liver markers (AST, ALT, ALP & total bilirubin) was predictive of complication (Table VII).
Table V: Graft (Hepatectomy) Type and complications.
|
Graft
|
No complications
|
Grade I
|
Grade II
|
Grade III&IV
|
P value
|
|
Right
|
45
|
14
|
7
|
5
|
0.514
|
|
Right
with MHV
|
6
|
3
|
1
|
2
|
|
Left
|
8
|
0
|
0
|
3
|
|
Left
lateral sector
|
3
|
0
|
0
|
0
|
|
Abandoned
|
2
|
1
|
0
|
0
|
|
Total
|
64
|
18
|
8
|
10
|
Table VI: The impact of MHV-inclusion
|
Graft
|
Right
|
Right with MHV
|
P value
|
|
No
|
45
|
6
|
0.672
|
|
Grade
I
|
14
|
3
|
|
|
Grade
II
|
7
|
1
|
|
|
Grade
III&IV
|
5
|
2
|
|
|
Total
|
71
|
12
|
|
Table VII: Spearman correlation coefficient of liver enzymes & total bilirubin with complications.
|
Test
|
Spearman correlation coefficient
|
p-value
|
|
AST
|
0.103
|
0.308
|
|
ALT
|
0.158
|
0.116
|
|
ALP
|
0.021
|
0.836
|
|
Total
bilirubin
|
-0.035
|
0.730
|
Discussion
The shortage of liver donation coupled with a high mortality rate of recipient on transplantation waiting list has resulted in temptations to extend donor criteria for liver donation (e.g. age>55, BMI>30, up to 30% hepatosteatosis, FLR<30%). (7) Such temptations should be balanced by perfect donor outcomes with minimal morbidity and no mortality of these volunteers.
Donor morbidity rate worldwide is estimated at 25-40% with around 0.2-0.5 % mortality.(8) Although most complications are minor, they result in prolongation of hospital stay, exaggeration of cost and poor overall donor satisfaction.(9-10) Our outcomes are comparable to published data with 36% overall morbidity rate and 10% major complication rates. 7 complications were completely preventable (6 caval clamp failures and one respiratory failure attributed to anesthesia).
Standardized and transparent reporting of adverse donor outcomes is of paramount importance and continuous clinical auditing is warranted.(11-12) The Clavien-Dindo classification of postoperative complications has been validated for liver transplantation and allows simple reproducible reporting of all complications.
Researchers have tried to identify modifiable risk factors of complications in donor hepatectomy but till now no such factor exist since donors are typically healthy individuals with no comorbidities.
Older age, higher BMI, both male and female genders, surgical experience and smaller FLR have all been suggested as risk factors.
In this study, we have found that older age is associated with increased risk of development of major grade III and IV complications. This may be partly related to a reduced regenerative capacity of the liver as suggested by many studies.(13-14)
A higher mean BMI was found in patients who develop all grades of complication. Obesity is well known risk factor for postoperative pulmonary, wound and thromboembolic complications as well as incisional hernia. In donor hepatectomy this is even exaggerated by the use of big J-shaped subcostal incision and prolonged operative time. It is also a marker of hepatosteatosis which impairs the regenerative capacity of the liver and may lead to prolonged postoperative cholestasis in the donor and delayed primary function in the recipients. Obese potential donors should be avoided or else should be offered a dietician consult followed by reevaluation after successful weight loss. In these donors liver biopsy for evaluation of hepatosteatosis is mandatory. (15-16)
The future liver remnant (equals estimated total liver volume- estimated graft volume/ total liver volume) is a major determinant of outcome after any hepatectomy. A FLR>25% is considered the lowest safety margin for resection of normal liver. This may be applicable for patients with malignant liver tumors since the benefit outweighs the risk and should not be generalized to donor hepatectomy where the donor has no direct benefit from the operation(16-18).The lack of correlation between FLR and out come in our study is mostly due to strict selection of donors. Potential donors with an estimated FLR <30% as measured by CT scan are rejected. 6 donors in our study had FLR <30% after hepatectomy (i.e. estimated total liver volume – weight of graft). 3 of these had minor complications and none developed major type III & IV complications. Compared to the whole cohort this was insignificant (p-value as calculated by Chi-square test 0.674).
Neither the type of the graft nor inclusion of MHV in right hepatectomy was found to adversely affect donor outcome. This finding however should be cautiously taken since only 12 right hepatectomies with MHV, 11 left hepatectomies and 3 left lateral sectorectomies were included in this study. This mandates future studies including more donors who undergo left donor hepatectomies. (19-21)
Although some studies have found a positive correlation between complications and preoperative alkaline phosphate test ALP and total bilirubin level(22) we have not found any correlation between routinely measured liver enzymes or total bilirubin and occurrence of complications. Actually, we do not accept donors with abnormal liver biochemical tests and our finding is in concordance with most studies published on this issue. (23-24)
Conclusion
Strict donor selection and meticulous surgical procedure remain the only modifiable factors to avoid complications after donor hepatectomy(25). Presence of more than one risk factor (older age, higher BMI, hepatosteatosis, expected FLR<30%) in a potential donor may be considered as relative contraindication to liver donation. Continuous transparent clinical audit of outcome is mandatory to identify potentially preventable adverse outcomes.
References
1.Strong RW, Lunch SV, Ong TH, et al. Successful liver transplantation from living donor to her son. NEJM 1990; 322: 1505-7.
2.Marsh JW, Gray E, Ness R, et al. Complications of right lobe living donor liver transplantation. J Hepatol 2009; 51: 715–24.
3.Yang X, Gong J, Gong J. The value of living donor liver transplantation. Ann Transplant 2012; 17: 120-4.
4.Barr ML, Belghiti J, Villamil FG, et al. A Report of the Vancouver Forum on the Care of the Live Organ Donor: Lung, Liver, Pancreas, and Intestine Data and Medical Guidelines. Transplantation 2006; 81: 1373-85.
5.Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo Classification of Surgical Complications: Five-Year Experience. Annals of Surgery 2009; 250: 187-96.
6.Tamura S, Sugawara Y, Kaneko J, et al. Systematic grading of surgical complications in live liver donors according to Clavien’s system. Transpl Int 2006; 19: 982-7.
7.Dirican A, Ozsoy M, Ates M, et al. Consequences of the Use of Extended Criteria Donors in Living Donor Liver Transplantation. Ann Transplant 2015; 20: 211-7
8.Cheah YL, Simpson MA, Pomposelli JJ, Pomfret EA. Incidence of Death and Potentially Life Threatening Near-Miss Events in Living Donor Hepatic Lobectomy: A World-Wide Survey. Liver Transpl 2013; 19: 499–506.
9.Hall EC, Boyarsky BJ, Deshpande NA, et al. Perioperative Complications After Live-Donor Hepatectomy. JAMA Surgery 2014; 149: 288-91
10.Lei J, Yan L, Wang W. Donor Safety in Living Donor Liver Transplantation: A Single-Center Analysis of 300 Cases. PLoS One 2013; 8(4): e61769.
11.Azoulay D, Bhanguia P, Andreania P, et al. Short- and Long-term Donor Morbidity in Right Lobe Living Donor Liver Transplantation: 91 Consecutive Cases in a European Center. Am J Transplant 2011;11:101-10.
12.Adcock L, Macleod C, Dubay D, et al. Adult Living Liver Donors have Excellent Long-Term Medical Outcomes: The University of Toronto Liver Transplant Experience. Am J Transplant 2010 ;10:364-71.
13.Patel S, Orloff M, Tsoulfas G, et al. Living-Donor Liver Transplantation in the United States: Identifying Donors at Risk for Perioperative Complications. Am J Transplant.2007; 7: 2344–49.
14.Yuan D, Wei YG, Li B, et al. Evaluation outcomes of donors in living donor liver transplantation: a single-center analysis of 132 donors. Hepatobiliary Pancreat Dis Int 2011; 10: 480-88.
15.Gruttadauria S, Pagano D, Cintorino D, et al. Right hepatic lobe living donation: A 12 years single Italian center experience. World J Gastroenterol 2013;19: 6353-59.
16.Guler N, Yaprak O, Gunay Y, et al. Major complications of adult right lobe living liver donors. Hepatobiliary Pancreat Dis Int 2015; 14: 150-6.
17.Hwang S, Lee SG, Lee YJ, et al. Lessons Learned From 1,000 Living Donor Liver Transplantations in a Single Center: How to Make Living Donations Safe. Liver Transpl 2006; 12:920-7.
18.Cho JY, Suh KS, Kwon CH, et al. Outcome of Donors with a Remnant Liver Volume of Less Than 35% After Right Hepatectomy. Liver Transpl 2006; 12: 201-6.
19.Dayangac M, Taner CB, Balci D, et al. Use of middle hepatic vein in right lobe living donor liver transplantation. Transpl Int 2010; 23: 285-91.
20.Uchiyama H, Shirabe K, Nakagawara H, et al. Revisiting the Safety of Living Liver Donors by Reassessing 441 Donor Hepatectomies: Is a Larger Hepatectomy Complication-Prone? Am J Transplant 2014;14:367-74.
21.Kousoulas L, Becker T, Richter N, et al. Living donor liver transplantation: effect of the type of liver graft donation on donor mortality and morbidity. Transpl Int 2011; 24: 251-8.
22.Ghobrial RM, Freise CE, Trotter JF, et al. Donor Morbidity After Living Donation for Liver Transplantation. Gastroenterology 2008; 135: 468-76.
23.Sun Z, Yu Z, Yu S, et al. Post-Operative Complications in Living Liver Donors: A Single-Center Experience in China. PLoS One 2015; 10(8): e0135557.
24.Abecassis MM, Fisher RA, Olthoff KM, et al. Complications of Living Donor Hepatic Lobectomy—A Comprehensive Report. Am J Transplant 2012; 12: 1208–17.
25.Wakade VA, Mathur SK. Donor Safety in Live-Related Liver Transplantation. Indian J Surg 2012; 74: 118-26.