ABSTRACT
Objectives: The aim of this study is to investigate the corresponding variables: age, sex, the reason for consultation, clinical manifestations, location, methods of diagnosis, time of surgery, type of surgery, histological diagnosis, the presence of infection and subsequent evolution, with baseline comparison of our findings to those reported in the literature.
Methods: A retrospective analysis carried out of the medical records of all the patients presented with spinal dermal sinuses cases treated surgically in our setup over a period of 10-years. From January 2005 to January 2015, at King Hussein Medical Center. The mean follow up was 87 months (14-109 months).
Results: The study group included 53 consecutive patients who were managed in a single center. Male : female ratio was 28:25. Mean age was 3.4 years, ranging from one month to 15 years. The mean follow up was 87 months (14-109 months). Anatomically the majority of the treated sinuses occurred in lumbar region 37-cases, representing 69.8 % of cases. 83% progressed satisfactorily.
Conclusion: Spinal dermal sinuses are a rare entity that may progress to a serious neurological condition. Early detection and management have good outcomes. The Paediatrician has a crucial role in diagnosis. Surgery aims to excise the sinus tract completely, excisable skin tags, and correct the dysraphic state in the same setting.
Keywords: Congenital, Inclusion tumour, Spinal dermal sinus.
JRMS Dec 2017; 24(3):43-47/DOI:10.12816/0042339
Introduction
Spinal dermal sinus is a rare congenital tubular tractanomaly, product of the incomplete separation between the neural ectoderm and the epithelial ectoderm during the first gestational weeks. It is a variety of dysraphism that allows a potential communication between the skin and the central nervous system (1) The inward extent of the tract traverses the underlying structures is variable, it may extend beyond the dura and terminate in the spinal cord or conus medullaris. It is located mostly in the midline, although apara-median location reported (2,3). It can originate at any level of the neuraxis, from the first cervical vertebra to the coccyx, most frequently in the lumbar region.The cutaneous stigmata that accompany the dermal sinus are a small hole or dimple, sometimes almost imperceptible, it may harbor suppuration, which may be accompanied by cutaneous angioma, hypertrichosis orsubcutaneous tumor. All of these findings are contemporaneous from birth (4)An inclusion tumor (dermoid cyst, Epidermoid cyst, or lipoma), can develop at any point of the length of the tract, more usually at the intra-dural level. These are produced by anomalous implantation of ectodermal cells during neural tube closure between the third and fifth weeks of embryonic life (4,5) As the intra-spinal portion of the sinus or the inclusion tumor is attached to the nervous structures, sinus ascends with them during the cephalic migration of the spinal cord, creating a long intra-dural trajectory between the cephalic end of the tract or cyst and the skin stigmata. Despite its harmless external appearance, they can produce serious neurological deficit and the treating physician has a crucial role in its early diagnosis. The objective of our work was to describe forms of presentation, diagnosis, and treatment of patients with dermal sinuses.
Methods
We carried out a retrospective analysis of the medical records of all the patients presented with spinal dermal sinuses cases treated surgically in our setup over a period of 10-years.The study group included 53 consecutive patients who were managed in a single centre, from January 2005 to January 2015.The purpose of this current study wasto investigate the corresponding variables: age, sex, the reason for consultation, clinical manifestations, location, methods of diagnosis, type of surgery, histological diagnosis, presence of infection and subsequent evolution.
Results
In our series of 53 treated patients, male: female ratio was 28:25. Mean age was 3.4 years, ranging from one month to 15 years. The mean follow up was 87 months (14-109 months). All our patients presented with an orifice which was the major complaint, other presentations are shown in Table I. Anatomically the majority of the treated sinuses occurred in lumbar region 37-cases, representing 69.8 % of cases, 9 cases in the cervical region and 7 cases in the dorsal region. Topographic localization was compared to reported literature Figure1. Stigmata associated with the spinal dermal sinuses shown in Table II. The histological diagnosis was of pure dermal in 39.6% of cases (n =21), 26.4% (n = 14) were associated with epidermoid cysts,17% (n = 9) with dermoid cysts and 17% (n = 9) with lipomas. All patients were clinically monitored with an average follow-up of 3.9 years, with MRI performed for follow up in those with surgically verified intra-dural component, inclusion tumor, or change in clinical picture. All evolved favorably with neurological examination, except 6-cases, that persisted with neurogenic deficit. Three cases developed para-paresis. The study group included 53 consecutive patients who were managed in a single center. Male: female ratio was 28:25. Mean age was 3.4 years, ranging from one month to 15 years. The mean follow up was 87 months (14-109 months). Anatomically the majority of the treated sinuses occurred in lumbar region 20-cases, representing 37.73 % of cases. 83% progressed satisfactorily.
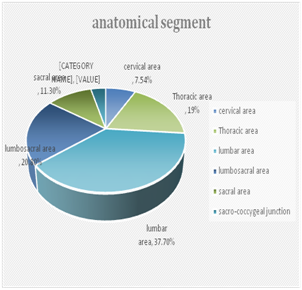
Figure.1:Topographic localization of spinal dermal sinus
Table I : Clinical characteristics of all patients at presentation
|
Manifestations
|
Number of cases
|
Percentage
|
|
Orifice
|
53
|
100%
|
|
Asymptomatic
|
34
|
64.2%
|
|
Neurological
deficits
|
19
|
35.8%%
|
|
Infection
|
4
|
7.5%
|
Table II: Cutaneous findings associated with dermal sinus.
|
Findings
|
Patients
|
Percentage
|
|
Sinus
ostea with a cephalically oriented tract
|
53
|
100%
|
|
Angiomata
|
5
|
9.4%
|
|
Hypertrichosis
|
15
|
28.3%
|
|
Skin
tags
|
12
|
22.6%
|
|
Abnormal
pigmentation
|
11
|
20.8%
|
|
Subcutaneous
lipomas
|
8
|
15.1%
|
DISCUSSION
The spinal dermal sinus is a rare entity; estimated incidence about one in every 2500 live births, it is always above the sacro-coxygeal level (4,7) It must be differentiated from another frequent entity; the sacro- coxygeal sinus, which is present in 2 to 4% of all newborns at the upper end of the fold and ends in the cases of maximum extension in the periosteum of the coccyx. These sinuses end blindly with no extension so it is not necessary to perform a radiological evaluation. The operation only needed if the background of the sinuses not displayed, to prevent future infections (1) Many publications on spinal dermal sinuses, emphasized that despite their benign external appearance, these lesions are capable of producing serious neurologic deficits disease due to meningitis, spinal cord compression, and infected dermoid cysts, as occurred in a large part of our cases (5-9) Medical records of our patients with dermal sinuses were analyzed and revealed 53-cases.All had a cutaneous orifice in the mid line Figure 2 . Regarding the anatomical segment involved our results compared to what has been reported in the literature (3,10 ,15) Results are shown in the chart Figure1. In terms of radiological evaluation, cutaneous stigmata and, or congenital anomalies often prompt screening, in all patients. Plain radiographs of the spine performed as the primary imaging modality (where dysraphy was not always found). All patients underwent magnetic resonance imaging, while in 7cases computed tomography (CT) was performed to further assess bone deformities (16-19) Magnetic resonance imaging showed the pathology, congenital anatomical abnormality and the tract in all cases Figure3. The surgery aimed to excise the sinus tract completely, excisable skin tags, and correct the dysraphic state in the same setting (2,20,21) Surgical steps were common for all the cases. The procedure included tracing, sinus tract through the subcutaneous tissue and muscle layer still its attachment with the neural axis. Tract excised completely. In cases where sinus was intradural, dura opened for further complete resection. Associated Intraspinal epidermoid, myelocele, pathologies; lipomeningomyelocele, abscess, arachnoid adhesion, tethered cord were dealt with accordingly (21,24) Those patients presenting with infectious complications were managed with appropriate antibiotics, after recovery surgery for resection of sinus, and correction of associated anomalies was performed. Our diagnostic and therapeutic algorithm specified in Figure 4 applied. Clinical outcome in most patients was excellent, 83% progressed satisfactorily regarding neurological examination, and on the other hand, 6-cases persisted with a neurogenic deficit. In addition, 3-cases developed para-paresis. Detailed clinical outcomes showed in Table III.

Figure 2: showing a lumbar spinal dermal Sinus Associated with massive lipoma
Figure 3: Thoraco-lumbar MRI, T2-wighted, sagittal view, showing a sacral spinal dermal sinus
Table III: Patient clinical outcome post-operatively
|
Patient Outcome
|
cases
|
percentage
|
|
Neurologically
intact pre- and postoperatively
|
34
|
39%
|
|
Had complete neurological recovery
|
10
|
17%
|
|
Neurologically unchanged
|
6
|
11.3%
|
|
Neurologically worsened
|
3
|
5.7%
|
Figure 4: Diagnostic and Therapeutic Algorithm
Conclusion
Spinal dermal sinuses despite their rarity and innocent appearance, may progress to a serious neurological condition. Early detection and management have favorable results. The Pediatrician has a crucial role in diagnosis. The surgery aims to excise the sinus tract completely, excisable skin tags, and correct the dysraphic state in the same setting.
References
1. French BN. The embryology of spinal dysraphism. ClinNeurosurg.1983;30:295–340
2. Iskandar BJ, Oakes WJ: Anomalies of the spine and spinal cord. In:McLone DG, ed. Pediatric Neurosurgery: Surgery of the Developing NervousSystem. Philadelphia, PA: WB Saunders Company; 2001:307–324.
3. Carrillo R, Career L, Prada J, Roses C. LateralCongenital spinal dermal sinus. ChilNervSyst1985; 1: 238-240.
4. Ackerman LL, Menezes AH, Follett KA. Cervical and thoracic dermal sinus tracts. A case series and review of the literature. PediatrNeurosurg. 2002. 37: 137-47.
5. Kaufman BA. Neural tube defects. PediatrClin North Am. 2004. 51: 389-419
6. Mete M, Umur AS, Duransoy YK, Barutçuoglu M, Umur N, Gurgen SG. Congenital dermal sinus tract of the spine: Experience of 16 patients. J Child Neurol. 2014. 29: 1277-82.
7. Radmanesh F, Nejat F, El Khashab M. Dermal sinus tract of the spine. Childs Nerv Syst. 2010. 26: 349-57
8. Ramnarayan R, Dominic A, Alapatt J, Buxton N. Congenital spinal dermal sinuses: Poor awareness leads to delayed treatment. Childs Nerv Syst. 2006. 22: 1220-4.
9. Zuccaro G, Sosa F, Monges J. Dermal sinuses Spinal Rev Argent Neurosurgery 1995; 9: 144-147.
10. Powell KR, Cherry JD, Hougen TJ, Blinderman EE, Dunn MC. A prospectivesearch for congenital dermal abnormalities of the craniospinal axis. J Pediatr. 1975;87:744–750.
11. McIntosh R, Merritt KK, Richards MR, Samuels MH, Bellows MT. Theincidence of congenital malformations: a study of 5,964 pregnancies.Pediatrics. 1954;14:505–521
12. Mount LA. Congenital dermal sinuses: as a cause of meningitis, intraspinalabscess and intracranial abscess. JAMA. 1949;139:1263–1268.
13. McComb JG: Congenital dermal sinus. In: Pang D, ed. Disorders of thePediatric Spine. New York, NY: Raven; 1995:349–360
14. Park TS, Kanev PM, Henegar MM, Kaufman BA. Occult spinal dysraphism.Neurol Surg. 1997;2:873–889.
15. Ingraham F, Matson D. Neurosurgery of infancy And childhood. 1st ed. Illinois: Charles Thomas,1954: 69-82.
16.Naidich TP, Harwood-Nash DC, McLone DG. Radiology of spinal dysraphism. ClinNeurosurg. 1983. 30: 341-65.
17. Cakmakci E, Cinar HG, Uner C, Ucan B, Eksioglu AS, Pala M, et al. Ultrasonographic clues for diagnosis of spina bifida occulta in children. Quantitative imaging in medicine and surgery. 2016;6(5):545-51.
18. Lee SM, Cheon JE, Choi YH, Kim IO, Kim WS, Cho HH, et al. Limited Dorsal Myeloschisis and Congenital Dermal Sinus: Comparison of Clinical and MR Imaging Features. AJNR American journal of neuroradiology. 2017;38(1):176-82.
19. O'Neill BR, Gallegos D, Herron A, Palmer C, Stence NV, Hankinson TC, et al. Use of magnetic resonance imaging to detect occult spinal dysraphism in infants. Journal of neurosurgery Pediatrics. 2017;19(2):217-26.
20. Calvit M, Guzman A. Timing of surgery in patients With infected spinal dermal sinuses. Child NervSyst 1995; 11: 129-132.
21. Lunardi P, Mossori P, Gagliardi F, Fortuna A. Long-term results of the surgical treatment of Spinal dermoid and epidermoid tumors. Neurosurg1989; 25: 860-864.
22. Kanev PM, Park TS. Dermoids and dermal sinus tracts of the spine.NeurosurgClin North Am. 1995;6:359–366
23. Gupta DK, Shastank RR, Mahapatra AK. An unusual presentation of lumbosacral dermal sinus with CSF leak and meningitis. A case report and review of the literature. PediatrNeurosurg. 2005. 41: 98-101.
24. Martínez-Lage J, Esteban J, Poza M, Casas C. Congenital dermal sinus associated with an Abscessed intramedullary epidermoid cyst inChild: case report and review of the literature.ChildNervSyst 1995; 11: 301-305.1.