ABSTRACT
Objectives: Primary spinal tumors arise from the different elements of the central nervous system; they originate from the spine cord itself and its adjacent structures. They are relatively one of the rarest pathologies.
In this analysis, authors aim to review the surgically treated cases of primary spinal cord tumors, to clarify the relative frequencies of these tumors, treated in our setup over a period of 15-years at King Hussein Medical Center. Special emphasis devoted to analyze the clinical manifestations, radiological findings, histological subtypes, anatomical location, and the mid-term outcome following surgery of these lesions.
Methods:This study was conducted by reviewing retrospectively the: patient's admission records, neuroimaging, operation records, outpatient files, histopathology reports and clinical outcome documents which were compiled from all consecutive patients treated in single referral center, between January 2002 and January 2017.
Results: In a cohort of 414-patients with primary spinal cord tumors surgically treated during the period of this study. The majority of the patients were male representing 58.21% of patients. The mean age at surgery was 53.6-years.Anatomically; there were 144-patients with intramedullary tumors, 181-patients (43.71 %), with intradural extramedullary tumors, 77-patients (18.59 %) with epidural tumors, and 12-patients (2.89 %) with dumbbell tumors. The pathological diagnoses of the primary spinal cord tumors are classified based on the age of the patient, the anatomic location of the lesion, supplemented by modern imaging and tumor histology.
Conclusion: Primary spinal cord tumors are remarkably rare. The recent surgical result of pain relief, neurological improvement, and local control rates suggest that surgery is effective in the treatment of patients with primary spinal tumors with minimal deterioration and complication rate. The most reliable predicting factor of postoperative neurological outcome is the preoperative neurological state.
Keywords: Extramedullary spinal tumor, Intradural, Outcome, Spine tumors.
JRMS December 2018; 25(3):39-44/ DOI: 10.12816/0552731
Introduction
Primary spinal tumors arise from the different elements of the central nervous system; they originate from the spinal cord itself and its adjacent structures (1). They are relatively one of the rarest pathologies, demonstrating about 4–16 % of all tumors arising from the central nervous systems according to former reports (2-5).They occur far infrequently than metastatic spinal tumors. Anatomically, these neoplasms may be categorized according to the compartment of origin (Table. I)
either intramedullary (inside the cord) or extramedullary (outside the cord), making them anatomically distinct from metastases which are special emphasis devoted to analyze the clinical manifestations, radiological findings, histological subtypes, anatomical location, vertebral level and the mid-term outcome following surgery of these lesions in patients who were managed at our center with baseline comparison of similarities and differences with those reported in literature.
Table I: Classification of Spinal Tumors by Location.
|
Extradural
|
Metastatic (carcinoma, lymphoma, melanoma, sarcoma), chordoma, epidermoid,
teratoma, dermoid, lipoma
|
|
Intradural
Extramedullary
Intramedullary
|
Nerve sheath tumors
(schwannoma), epidermoid, teratoma, dermoid, lipoma, neurenteric cyst
Astrocytoma,
ependymoma, hemangioblastoma
|
Methods
This study was conducted by reviewing retrospectively the: patient's admission records, neuroimaging, operation records, outpatient files, histopathology reports and clinical outcome documents which were compiled from all consecutive patients treated in single referral center. Patient data were extracted from the KHMC Primary Spinal Tumors electronic Database, between January 2002 and January 2017.We analyzed data from 414-patients who underwent surgery for a single spinal cord tumor confirmed by histopathological examination. In each case, collected data included demographic features; sex, age, size of the tumor, the anatomical location of tumors (intramedullary, intradural extramedullary, epidural and dumbbell), the vertebral level location (cervical, cervicothoracic, thoracic, thoracolumbar, lumbar, lumbosacral and sacral), the resection extent, histological alterations, local recurrence, perioperative morbidity, and complications were documented. Preoperative radiological imaging reports were used to confirm tumor location and size based on largest single dimension. The extent of resection was based upon surgical operative notes and post-operative imaging.
Surgical technique
After a detailed preoperative diagnostic evaluation, patients were managed surgically via partial or total laminectomy proximal to the marked pathology through a posterior approach (Figure. 1). The Cardinal aim in all cases was the maximum safe resection; also extra efforts were made to prevent postoperative instability.
Fig.1: Intraoperative images showing the steps of spinal tumor excision.
Results
Patient demographics: In a cohort of 414-patients with primary spinal cord tumors surgically treated during the period of this study. The majority of the patients were male representing 58.21% of patients (241-patients) and 41.30 % were female (171-patients). The mean age at surgery was 53.6-years (range, 16-years to 76-years). Only 4.58 % of patients were under 20-years of age.Anatomically, there were 144-patients (34.78 %) with intramedullary tumors, 181-patients (43.71 %), with intradural extramedullary tumors, 77-patients (18.59 %) with epidural tumors, and 12-patients (2.89 %) with dumbbell tumors (Fig. 2). With respect to the vertebral level where these tumors were located, they occurred mainly at the level of the thoracic spine (156-patients, 37.68%), followed by lumbar spine (120-patients, 28.98%), then thoraco-lumbar segment (50-patients, 12.07%) and cervical (39 patients, 9.42%) (Figure. 3).The pathological diagnoses of the primary spinal cord tumors are classified based on the age of the patient, the anatomic location of the lesion, supplemented by modern imaging and tumor histology, our results are shown in (Table.II).
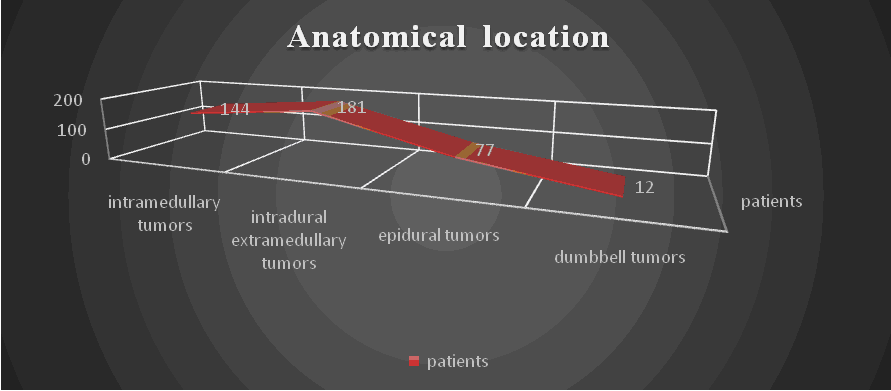
Fig.2: The anatomical distribution of spinal tumors.
Fig.3: The Segmental distribution of spinal tumors at various spinal vertebral levels.
Table II: Primary spinal cord tumors distribution by histology
|
Tumor
|
Number
|
|
Schwannoma
|
67
|
|
Ependymoma
|
63
|
|
Meningioma
|
87
|
|
Lipoma
|
59
|
|
astrocytoma
|
29
|
|
Hemangioblastoma
|
17
|
|
Epidermoid
|
12
|
|
Chordoma
|
9
|
|
dermoid
|
11
|
|
Neurofibroma
|
23
|
|
Others
|
37
|
Discussion
This study appraises the accumulative work of a single referral center, bestowing series of cases of primary spinal cord tumors in Jordan. Our study used the Patient data extracted from the KHMC Primary Spinal Tumors electronic Database to retrospectively scrutinize tumor cases. This work is a supplementary work to our previous publications (5.11,12).
The initial clinical presentation of patients with spinal tumors is commonly pain, also might be spinal deformity or neurologic deficit. Persistent and usually not related to activity back pain is the cardinal symptom. It is often intensifies during the night. Patients with spinal tumors rarely present with palpable mass.Spinal instability and neurologic compromise may ascend from a lesion in the vertebral body and depend on the level and location (13-16). This study showed that pain was the major cause provoked investigations; pain was localized, sharp in nature and mostly temporarily, due to the direct or indirect compression of the nerve root by the tumor in 271-cases. Later on, when compression increases to the spinal cord, spinal tracts get damaged and myelopathy developed in 158-cases.
The armamentarium of diagnostic work-up includes; laboratory investigations, radiology imaging studies (standard two planes radiographs, CT and MRI as well as a bone scan), and tumor staging with a biopsy from the lesion. Tumor staging delineates the local magnitude; the systemic extent of the disease; which is mandatory for surgical planning and should be done in accordance with the surgeon performing the tumor resection to allow the prognosis to be determined. Our center has all this modalities.MRI is the mainstay of the diagnosis in most of the cases.
The treatment intentions of primary spine tumors are directed towards local control achievement, which may not only alleviate symptoms, but may lead to considerable improvements in overall survival (17). The contemporary standard treatment for primary spine tumors depends mainly on the pathology of the tumor. When feasible, surgical resection is typically the treatment of choice (18-21) .In our center patients were managed surgically via partial or total laminectomy proximal to the marked pathology through a posterior approach. Indeed the cardinal aim in all cases was the maximum safe resection; also extra efforts were made to prevent postoperative instability. Anatomically, this review showed 144-patients (34.78 %) with intramedullary tumors, 181-patients (43.71 %), with intradural extramedullary tumors, 77-patients (18.59 %) with epidural tumors, and 12-patients (2.89 %) with dumbbell tumors (Figure. 1). Regarding the vertebral level these tumors occurred mainly at the level of the thoracic spine (156-patients, 37.68%), followed by lumbar spine (120-patients, 28.98%), then thoraco-lumbar segment (50-patients, 12.07%) and cervical (39 patients, 9.42%) (Figure.2). Our institution’s study showed that surgical intervention provides good clinical response regarding: pain; neurological improvement and local tumor control. Pain control was the main role of surgery with response rate of 88% suggests surgical intervention is effective in achieving pain relief in patients with primary spine tumors. Neurological improvement was also observed in 65%.The most notable complications observed in this series include 6-patients who developed a progression of proximal lower extremity weakness, while CSF leak observed in 11-cases and infection of surgical site in 8-patients.
Conclusion
Primary spinal cord tumors are remarkably rare. The recent surgical result of pain relief, neurological improvement, and local control rates suggest that surgery is effective in the treatment of patients with primary spinal tumors with minimal deterioration and complication rate.The most reliable predicting factor of postoperative neurological outcome is the preoperative neurological state.
Study limitations:
Limitations of this study include those that are inherent in retrospective analyses. Another limitation of our study is the small sample size, which is difficult to overcome due to the low incidence of primary spine tumors with diverse tumor types. To the best of our knowledge, our series is one of the largest to date focusing on the response of primary spine and spinal cord tumors treated at a single institution with treatment uniformity and consistent reporting of clinical responses.
References
1-Ciftdemir M, Kaya M, Selcuk E, Yalniz E. Tumors of the spine. World journal of orthopedics. 2016;7(2):109-16.
2-Hirano K, Imagama S, Sato K, Kato F, Yukawa Y, Yoshihara H, et al. Primary spinal cord tumors: review of 678 surgically treated patients in Japan. A multicenter study. European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2012;21(10):2019-26.
3-Liigant A, Asser T, Kulla A, Kaasik AE. Epidemiology of primary central nervous system tumors in Estonia. Neuroepidemiology. 2000;19:300–311.
4-Suh YL, Koo H, Kim TS, Chi JG, Park SH, Khang SK, Choe G, Lee MC, Hong EK, Sohn YK, Chae YS, Kim DS, Huh GY, Lee SS, Lee YS. Tumors of the central nervous system in Korea—a multicenter study of 3221 cases. J Neurooncol. 2002;56:251–259.
5-Alqroom RY, Abu-nowar HA, Shaban FA, Alqurashi MR, Khraisat WM, Al ShurbajiAA.Spinal Schwannoma: scrutinizing the armamentarium of a single institute.JRMS April 2018; 25(1):50-55.
6-Schellinger KA, Propp JM, Villano JL, McCarthy BJ: Descriptive epidemiology of primary spinal cord tumors. Journal of neuro-oncology 2008, 87(2):173-179.
7-Ropper AE, Cahill KS, Hanna JW, McCarthy EF, Gokaslan ZL, Chi JH: Primary vertebral tumors: a review of epidemiologic, histological, and imaging findings, Part I: benign tumors. Neurosurgery 2011, 69(6):1171-1180.
8-Ropper AE, Cahill KS, Hanna JW, McCarthy EF, Gokaslan ZL, Chi JH: Primary vertebral tumors: a review of epidemiologic, histological and imaging findings, part II: locally aggressive and malignant tumors. Neurosurgery 2012, 70(1):211-219.
9-Duong LM, McCarthy BJ, McLendon RE, Dolecek TA, Kruchko C, Douglas LL, Ajani UA: Descriptive epidemiology of malignant and nonmalignant primary.
10-spinal cord, spinal meninges, and cauda equina tumors, United States, 2004-2007. Cancer 2012, 118(17):4220-4227.
11-Alqroom Rami, Fayyad Luma, Abu Salma Zuhair,Ma'ayaAlhareth, Al-loziRakan, Al Shurbaji Amer. Demographics & Inferences of Spinal Meningioma. IJSR2017; 6(5):348-50.
12-KhasawnehNidal, Alqroom Rami, Sha'ban Firas, Al DrousRafeed, Nserat Rima, AlShurbaji Amer.Congenital Spinal Lipoma: analyzing the perplexed nomenclature and our management.JRMS August 2018; 25(1):50-55.
13-Hori T, Takakura K, Sano K. Spinal neurinomas--clinical analysis of 45 surgical cases. Neurol Med Chir (Tokyo) 1984;24:471–477.
14-Subaciute J. [Early diagnosis of spinal cord schwannoma : the significance of the pain syndrome] Medicina (Kaunas) 2002;38:1086–1088.
15-Lot G, George B. Cervical neuromas with extradural components: surgical management in a series of 57 patients. Neurosurgery. 1997;41:813–822.
16-Dorsi MJ, Belzberg AJ. Paraspinal nerve sheath tumors. Neurosurg Clin N Am. 2004;15:217–222.
17-Wong DA, Fornasier VL, MacNab I. Spinal metastases: the obvious, the occult, and the impostors. Spine. 1990;15(1):1-4.
18-Elibe E, Boyce-Fappiano D, Ryu S, Siddiqui MS, Lee I, Rock J, et al. Stereotactic radiosurgery for primary tumors of the spine and spinal cord(dagger). Journal of radiosurgery and SBRT. 2018;5(2):107-13
19-Engelhard HH, Villano JL, Porter KR, Stewart AK, Barua M, Barker FG, et al. Clinical presentation, histology, and treatment in 430 patients with primary tumors of the spinal cord, spinal meninges, or cauda equina. Journal of neurosurgery Spine. 2010;13(1):67-77.
20-Mukherjee D, Chaichana KL, Adogwa O, Gokaslan Z, Aaronson O, Cheng JS, et al. Association of extent of local tumor invasion and survival in patients with malignant primary osseous spinal neoplasms from the surveillance, epidemiology, and end results (SEER) database. World neurosurgery. 2011;76(6):580-5.
21-Mukherjee D, Chaichana KL, Gokaslan ZL, Aaronson O, Cheng JS, McGirt MJ. Survival of patients with malignant primary osseous spinal neoplasms: results from the Surveillance, Epidemiology, and End Results (SEER) database from 1973 to 2003. Journal of neurosurgery Spine. 2011;14(2):143-50.