ABSTRACT
Objective: To present our
experience and evaluate the safety of our approach for the management of
children with a pulseless hand secondary to supracondylar fracture of the
humerus (SHF).
Methods: A retrospective
study was conducted at the vascular surgery department and orthopedic
department at King Hussein Medical Center (KHMC).
Pediatric patients that presented to ( KHMC) with (SHF) and a
pulseless hand between April 2016 and April 2018 were included in the study.
Data included the patients’ age, sex, time between trauma and presentation,
signs of hand ischemia, resumption of pulses after fracture reduction,
necessity for surgical exploration, type of vascular injury and intervention,
outcomes of the vascular repair, and ischemic sequelae.
Results: 160 patients
with SHF were admitted to KHMC during the study, of which 23 had an absent
pulse. The age range of the patients was 3-14 years, (mean 6.3 years, SD
2.87).The time interval between the trauma and presentation to KHMC was 2-25
hours (mean 5.13 hours, SD 4.99). 5 of the 23 patients had signs of hand
ischemia, 18 of the 23 had a pulseless but perfused hand.
Overall, 19 of the patients 23 (82.6%) underwent brachial artery
exploration; 5 of 19 (26.32%) underwent brachial thrombectomy; 6 of 19 (31.58%)
underwent brachial artery mobilization followed by thrombectomy; 5 of 19 (26.32
%) underwent brachial artery repair using saphenous vein graft; and 3 of 19
(15.78%) underwent stripping of the brachial artery adventitia followed by
thrombectomy.
There were no
cases of amputation, fasciotomy, re-exploration, or long-term ischemic
complications.
Conclusion:
Early brachial artery exploration is recommended in padiatric
patients with SHF and pulseless hand to prevent limb loss and debilitating
long-term ischemic complications.
Keywords: Supracondylar fracture, pulseless hand, pediatric, brachial.
JRMS December 2019; 26(3):28-36/ DOI: 10.12816/0054815
Introduction
Supracondylar fracture of the humerus (SHF) is a common childhood injury, accounting for up to 70% of all pediatric elbow fractures. 1, 2, 8,9,10, The incidence of vascular injury in pediatric SHF has been reported to range between 3-14%.3,5,8 Brachial artery lesion may be secondary to various mechanisms, including entrapment in the fracture, transection , vasospasm, and contusion with thrombus formation 5,6. If not detected and properly managed, brachial artery injury could lead to serious ischemic complications such as amputation and Volkmann’s contracture 1, 3, 9.
Falling onto an outstretched hand with a hyperextended elbow is the most common mechanism of injury and usually results in displacement of the distal portion of the humerus.3, 10, 11. Neurovascular structures are in close proximity to the elbow joint and are vulnerable to injury in this type of fracture. 2, 4
SHF in children are classified into three grades according to the Gartland classification which was presented in 1959, grade III being the most severe, and the most likely to be associated with vascular injury 4,5,12, .(Fig.1&2) show examples of grade III gartland fractures . Complications of these fractures include infection, loss of fracture reduction, non-union, cubitus varus or valgus, and neurovascular injury.6, 7, 12
The incidence of vascular injury in pediatric SHF has been reported to range between 3-14%.3,5,8 Brachial artery lesion may be secondary to various mechanisms, including entrapment in the fracture, transection , vasospasm, and contusion with thrombus formation 5,6. If not detected and properly managed, brachial artery injury could lead to serious ischemic complications such as amputation and Volkmann’s contracture 1, 3, 9.
Although immediate brachial artery exploration in the case of a pulseless, cold, ischemic hand is a widely accepted approach, the management of patients with a pulseless pink hand after successful fracture reduction and fixation continues to be debated and no clear therapeutic approach exists.
The aim of this study was to describe our approach in the management of a pulseless hand after grade III SHF in children. The primary end result was resumption of distal pulses after brachial artery exploration.
Materials and Methods
This is a retrospective study that was conducted at the vascular surgery department and orthopedic department in King Hussein Medical Center (KHMC), Amman- Jordan.
The study included all pediatric patients who presented or were referred to KHMC with (SHF) and a pulseless hand between April 2016 and April 2018. Data was collected from operation room records, patients’ records, and vascular laboratory records. Data included the patients’ age, sex, time interval between trauma and presentation, the presence of signs of hand ischemia, resumption of pulse after fracture reduction, the necessity for surgical exploration, type of vascular injury, type of vascular intervention, outcomes of vascular repair, and ischemic sequelae.
The type of fracture was assessed by anteroposterior (AP) and lateral X-rays of the elbow before and after fracture reduction and was classified according to Gartland classification.
All patients with a (SHF) and suspected vascular injury were assessed by a vascular surgeon in the emergency room and after reduction of the fracture. This included assessment of hand pulse status (radial and ulnar pulses), hand color and temperature, capillary refill time, and arterial signals by hand-held Doppler (HHD).
Our approach was to proceed with immediate brachial artery exploration for patients with a pulseless cold ischemic hand. Patients with a pulseless pink hand underwent closed reduction under fluoroscopy, followed by percutaneous fixation with Kirschner wires (K-wires). If the pulse did not return after fracture reduction, we proceeded with early brachial artery exploration (in the same session).
For patients that needed arterial exploration (Those with ischemic hand or failure to resume pulse after fracture reduction), unfractionated heparin was given as a bolus dose according to body weight (80 IU /KG ) followed by a maintenance dose of ( 18 IU /KG/H), with dose adjustment according to the activated partial thromboplastin time(APTT) ; the target APTT was two times above its
normal range of 35–42 seconds .
The standard incision was a longitudinal one over the anteromedial aspect of the elbow region. Arterial procedures which were performed included simple embolectomy, release from entrapment, and repair using vein interposition. All surgeries were performed under general anesthesia with antibiotic prophylaxis. All patients were followed monthly in the vascular surgery clinic for a minimum of six months.
Since this is a retrospective study, and data were already collected; we used a post hoc power analysis. A post hoc power analysis was conducted using the G Power software (Faul and Erdfelder 1992). We have done a post hoc power analysis based on the sample collected. The used sample (N=160) achieved 99% power at a 5% level of significance with small effect (f 2 = .02)
The statistical package for social sciences version 21 was used for analysis of the data. Mean and standard deviation values were calculated for numerical data such as age and time between trauma and presentation. Frequency and percentage values were calculated for the sex of the patients.
Result
During the study period, 160 patients with SHF were admitted to KHMC; 11 of them were referred from other hospitals owing to a pulseless hand.
Of the 160 patients, (87) patients had (Gartland type I or 11 fractures). None of those patients showed clinical evidence of vascular injury, so they were excluded from our study. The other 73 patients had Gartland III fracture (extension type), of which 23 had an absent pulse. Five of the 23 patients had signs of hand ischemia (pale, cold hand, delayed capillary refilling, absent waveform, and saturation on pulse oximetry). The other 18 patients had a pulseless but perfused hand.
In the study, 15 of the 23 patients (65.22 %) were males and 8 of the 23 patients (34.78 %) were females, with a male to female ratio of 1:1.87.
The right side was affected in 14 of the 23 patients (60.87 %) whereas the left side was affected in 9 of the 23 (39.13%) patients (Table 1).
|
|
|
Table I:Demographics of the Included
Population (in percent).
|
|
Feature
|
n= 23
|
Total records %
|
|
Gender
|
|
|
|
Male
|
15
|
65.22%
|
|
Female
|
8
|
34.78%
|
|
Signs of hand ischemia
|
|
|
|
Present
|
5
|
21.74
|
|
Not Present
|
18
|
78.26
|
|
Affected Hand
|
|
|
|
Right hand
|
14
|
60.87
|
|
Left hand
|
9
|
39.13
|
|
Gartland type
|
|
|
|
Type I
|
0
|
0%
|
|
Type II
|
0
|
0%
|
|
Type III
|
23
|
100%
|
|
Absent pulse
|
|
|
|
Yes
|
23
|
100%
|
|
No
|
0
|
0%
|
|
|
The age range was 3 -14 years with a mean of 6.3 years (SD 2.87). The time interval between the trauma and presentation was 2-25 hours with a mean of 5.13 hours (SD 4.99), as summarized in Table II.
|
|
|
Table II:Descriptive Statistics of the
Patients’ Records (n = 23)
|
|
Feature
|
Mean
|
Standard deviation (SD)*
|
|
Age
|
6.30
|
2.87
|
|
Time between trauma
and presentation
|
5.13
|
4.99
|
|
*SD:Standard
deviation.
|
|
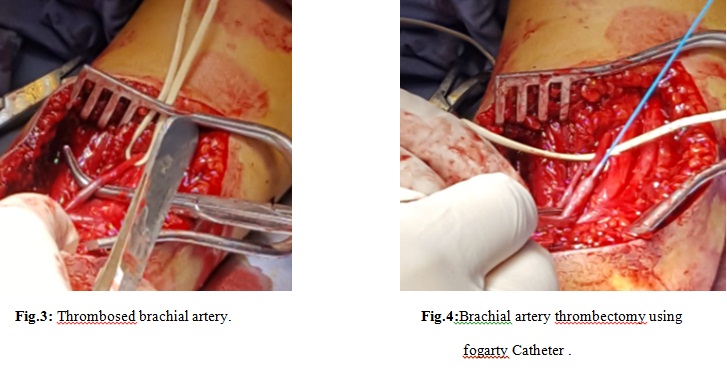
The 5 patients who presented with ischemic hand underwent immediate brachial artery exploration before fracture reduction to minimize the ischemia time and avoid any further arterial damage during fracture reduction. Two of them had an entrapped and kinked brachial artery with intraluminal thrombus; mobilization followed by thrombectomy was sufficient to resume a normal pulse. One patient had a complete transaction of the brachial artery, which was repaired by a reverse saphenous vein interposition graft. The remaining two patients had a thrombosed brachial artery with mild contusion; thrombectomy was performed, which resulted in successful resumption of normal distal pulses (Fig 3&4).
Fracture reduction and fixation was performed in the same setting after arterial procedure. All 5 patients had a palpable radial pulse at the completion of the surgery.
The 18 patients with a pulseless but perfused hand underwent closed reduction and fixation of the fracture by Kirshner wires. After fracture reduction, the pulses resumed in 4 patients. Those 4 patients underwent a duplex scan the next day, which confirmed the patency of the brachial, radial and ulnar arteries with a normal triphasic waveform.
The remaining 14 patients underwent brachial artery exploration in the same anesthesia setting. The intraoperative findings were brachial artery contusion with intraluminal thrombus in 5 patients, brachial artery entrapment and kinking in 4 patients, adventitial hematoma with an arterial spasm in 3 patients, and transection of the brachial artery in 2 patients. Of the 5 patients with contused and thrombosed brachial artery segment, 3 had resumption of radial pulse after simple brachial thrombectomy with smooth triphasic signals by the handheld Doppler. The other 2of the 5 patients needed replacement of the contused segment by reverse great saphenous vein graft because the injured brachial artery segment was severely damaged and thrombogenic. Normal distal pulses were resumed in all of them.
The four patients with arterial kinking underwent release of the artery followed by thrombectomy, with the resumption of distal pulses in all of them. The 3 patients with adventitial hematoma and spasm underwent partial stripping of the adventitia and thrombectomy to dilate the artery and relieve the spasm; all of them had palpable distal pulses at the completion of surgery.
The remaining two patients with brachial artery transection underwent successful repair using saphenous vein interposition because primary anastomosis was not feasible without excessive mobilization and potential loss of precious collaterals. The intraoperative findings and surgical procedures are summarized in Tables III, IV &V.
|
Table III :
Necessity for surgical exploration.
|
|
|
Necessity for surgical exploration
|
n= 23
|
Total records %
|
|
|
|
|
|
|
|
Brachial
artery exploration after fracture reduction.
|
14
|
60.87%
|
|
|
Immediate
brachial artery exploration
|
5
|
21.74%
|
|
|
Exploration
was not needed
|
4
|
17.39%
|
|
|
Table IV: Types of vascular injurie ( Intraoperative
findings).
|
|
|
Type of
vascular injury
|
n= 19
|
Total records%
|
|
Brachial artery entrapment and kinking.
|
6
|
31.58%
|
|
Adventitial hematoma with an arterial
spasm.
|
3
|
15.79%
|
|
Have thrombosed brachial artery
with contusion.
|
7
|
36.84%
|
|
Transection of the brachial artery .
|
3
|
15.79%
|
|
TableV:
Types of vascular interventions.
|
|
|
|
Type of
vascular intervention
|
n=
19
|
Total
records %
|
|
Thrombectomy
|
5
|
26.32%
|
|
Mobilization
followed by thrombectomy
|
6
|
31.58%
|
|
Reversed saphenous vein graft
Adventitial
stripping and thrombectomy
|
5
3
|
26.32%
15.78%
|
All patients were started on heparin infusion immediately after surgery for the whole in-patient period. All patients were discharged on aspirin for a minimum of three months with regular follow up in the vascular surgery clinic for a minimum of 6 months. None of the patients had ischemic complications or needed any further intervention.
Discussion
The purpose of this study was to describe our policy for the management of a pulseless hand after gartland type III SHF in children. Gartland type III SHF in children associated with vascular compromise should be considered as a surgical emergency. 2,9,11
Early surgical exploration of the cubital fossa before fracture reduction in patients with signs of acute ischemia is strongly recommended to minimize the ischemia time and avoid further arterial injury during the manipulation for fracture reduction. 9, 10, 13
The incidence of vascular injury in our study was 14.4 %. The diagnosis of vascular compromise was based on a clinical assessment because any other diagnostic tool would prolong the ischemia time, with added risks of radiation exposure and contrast agent toxicity.
We adopted immediate brachial artery exploration in a pulseless ischemic hand and early brachial artery exploration in all patients who did not resume distal pulses after fracture reduction in a pink perfused hand.
The management of a pink perfused pulseless hand in SHF in terms of vascular exploration is controversial, and consensus has not been established yet 1, 4, 10-16, 19.
According to the literature, several approaches have been proposed for the management of a pink pulseless hand. Some authors advise early brachial artery exploration and repair if distal pulses did not resume immediately or shortly after fracture reduction, even if the hand was pink and well-perfused 14-18.White et al.14 performed a systematic review of the literature for relevant studies of vascular injuries in pediatric SHFs and concluded that conservative management of pulseless and perfused hand needs to be questioned in the majority of published studies, because an absent pulse was associated with brachial artery injury in the majority of cases, even if the hand was pink and perfused. Moreover, outcomes of revascularization procedures were associated with high success rates, making this intervention worthwhile. Schoenecker et al. 15 reported their experience in early brachial artery exploration in seven patients that had a pulseless pink hand after SHF reduction. The patients were followed for an average of 30 months; all seven patients had normal perfusion status, including a radial pulse. Noaman 16 reported his experience with microsurgical repair of brachial artery injury in 31 pediatric patients with SHF who had an absent distal pulse after fracture reduction; 30 of the patients had excellent functional and perfusion status ,whereas one patient had Volkmann’s ischemic contracture that was subsequently treated by free functioning gracilis muscle transfer.
Blakey et al. 19, reported serious ischemic complications (Volkmann’s contracture) in 23 of 26 patients with type III SHF with a pink, pulseless and well-perfused hand that were initially treated by closed reduction without arterial exploration.The patients were referred to their institution at a mean period of three months after fracture. They recommended urgent neurovascular exploration in a pink pulseless hand after fracture reduction in all patients that have persistent and increasing pain, which is predictive of neurovascular injury.
Observation is also the treatment of choice for many authors 20-24. They prefer this approach because targeted vessels are often small in diameter and may require microsurgical expertise for reconstruction. Furthermore, brachial artery exploration may cause injury to collateral vessels that are important to maintain a viable limb, and there is significant risk of symptomatic re-occlusion and stenosis 22.
Louahem et al.5 recently published their experience, in which they reviewed 68 patients with pink pulseless hands among 404 Gartland III cases; they adopted urgent fracture reduction followed by close observation for hand perfusion and if any signs of ischemia or compartment syndrome develops. Immediate vascular exploration was performed only if signs of circulation disturbances developed. They concluded that a pulseless hand is not a strong indicator of arterial injury when the hand is perfused and warm.
Garbuz et al. 20 reported their experience with 5 patients that had a pink pulseless hand after fracture reduction, who were treated conservatively; none of the patients had any problems at the final review.
Malviya et al. 21 performed a review questionnaire study of pediatric orthopedic surgeons, which revealed that only 16.1% of surgeons would proceed to exploration of vessels if pulses remained absent after fracture reduction.
Our study showed that early brachial artery exploration is a safe approach. This practice was only possible because of the round-the clock availability of experienced vascular surgeons. In addition, this approach prevented the need for fasciotomy and decreases the possibility of long-term ischemic sequelae such as Volkmann’s ischemic contracture.
Conclusions
The absence of a distal pulse in children with SHF is strongly associated with brachial artery injury even if the hand is well-perfused. Early brachial artery exploration is recommended to prevent limb loss and debilitating long-term ischemic complications.
Acknowledgement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. We thank Zoran Dinev, PhD, from The Science Editorium (www.escienceeditorium.com) for editing a draft of this manuscript.
Ethical committee Approval:
Approval by the ethical committee of Jordanian Royal Medical Services was obtained before starting this research. Informed consent was not obtained as the study is retrospective in nature.
REFERENCES
1- Griffin KJ, Walsh SR, Markar S, Tang TY, Boyle JR, Hayes PD. The Pink Pulseless Hand: A Review of the Literature Regarding Management of Vascular Complications of Supracondylar Humeral Fractures in Children. Eur J Vasc Endovasc Surg (2008) 36: 697-702.
2- Korompilias A.V, Lykissas MG ,G. I. Mitsionis GI , Kontogeorgakos VA ,Manoudis G ,Beris AE. Treatment of pink pulseless hand following supracondylar fractures of the humerus in children. International Orthopaedics (SICOT) (2009) 33:237–241.
3- Usman R, Jamil M, Hashmi JS. Management of Arterial Injury in Children with Supracondylar Fracture of the Humerus and a Pulseless Hand. Ann Vasc Dis (2017) 10 (4) : 402–406.
4- Matuszewski L. Evaluation and management of pulseless pink/pale hand syndrome coexisting with supracondylar fractures of the humerus in children. Eur J Orthop Surg Traumatol (2014) 24:1401–1406.
5- Louahem D, Cottalorda J. Acute ischemia and pink pulseless hand in 68 of 404 gartland type III supracondylar humeral fractures in children: Urgent management and therapeutic consensus .Injury, Intl.J.Care Injured (2016) 47:848-852.
6- Leiblein M, Lustenberger T, Schulz AK, Rixen TS, Marzi I. Neurovascular complications after supracondylar humerus fractures in children. Trauma Case Reports (2017) 8: 16–19.
7- Mangat KS, Martin AG, Bache CE. The ‘pulseless pink’ hand after supracondylar fracture of the humerus in children,THE PREDICTIVE VALUE OF NERVE PALSY. J Bone Joint Surg (2009) 91:1521-1525.
8- Başbuğ HS , Göçer H, Özışık K. Surgical treatment of pulseless pediatric supracondylar humerus fracture. Int. J.Cardiovasc. Academy (2017) 3 :31-33.
9- Naziha T, Wan-Yuhana WMS ,Hadizie D, Paiman M, Abdul-Nawfar S, Wan-Azman WS, et al . Early Vessels Exploration of Pink Pulseless Hand in Gartland III Supracondylar Fracture Humerus in Children:Facts and Controversies . Malays Orthop J (2017) V 11 N 1.
10- Barr LV. Paediatric supracondylar humeral fractures: epidemiology, mechanisms and incidence during school holidays. J Child Orthop (2014) 8:167–170.
11- Brahmamdam P, Plummer M, Gregory M, Stephen M,
Clagett GP, Valentine RJ .Hand ischemia associated with elbow trauma in children. J Vasc Surg (2011) 54:773-778.
12- Oetgen M, Mirick G, Atwater L, Lovejoy J. Complications and Predictors of Need for Return to the Operating Room in the Treatment of Supracondylar Humerus Fractures in Children. The Open Orthop .J (2015) 9:139-142.
13- Helmut W, Robert E; Tanja K , Holger T , Christian E, Georg S. The impact of arterial vessel injuries associated with pediatric supracondylar humeral fractures. J. Trauma Acute Care Surg (2014), 77(2):381–385.
14- White L, Mehlman CT, Crawford AH. Perfused, Pulseless,and Puzzling: A Systematic Review of Vascular Injuries in Pediatric Supracondylar Humerus Fractures and Results of a POSNA Questionnaire.J Pediatr Orthop (2010), 30(4):328-335.
15- Schoenecker PL, Delgado E, Rotma M, Sicard GA, Capelli AM. Pulseless Arm in Association with Totally Displaced Supracondylar Fracture. J Orthop Trauma (1996), 10(6):410-415.
16- Noaman HH. Microsurgical reconstruction of brachial artery injuries in displaced supracondylar fracture humerus in children.Microsurgery (2006).26:498-505.
17- Badkoobehi H, Choi PD, Bae DS, Skaggs DL. Management of the Pulseless Pediatric Supracondylar Humeral Fracture. J Bone Joint Surg Am (2015). 97(11):937–943.
18- Luria S, Sucar A, Eylon S, Pinchas-Mizrachi R, Berlatzky Y, Anner H, et al. Vascular complications of supracondylar humeral fractures in children. J Pediatr Orthop (2007) .16(2):133-143.
19- Blakey CM, Biant LC, Birch R. Ischaemia and the pink, pulseless hand complicating supracondylar fractures of the humerus in childhood, long-term follow-up. J Bone Joint Surg (2009).91:1487-1492.
20- Garbuz DS, Leitch K, Wright LG. The treatment of supracondylar fractures in children with an absent radial pulse. J Pediatr Orthop (1996) 16:594–596.
21- Malviya A, Simmons D, Vallamshetla R, Bache CE .Pink pulseless hand following supra-condylar fractures: an audit of British practice. J Pediatr Orthop (2006), 15:62–64.
22- Sabharwal S, Tredwell SJ, Beauchamp RD, Mackenzie WG, Jakubec DM, Cairns R, et al .Management of pulseless pink hand in pediatric supracondylar fractures of humerus. J Pediatr Orthop (1997), 17:303–310.23
23- Choi PD, Melikian R, Skaggs DL. Risk Factors for Vascular Repair and Compartment Syndrome in the Pulseless Supracondylar Humerus Fracture in Children. J Pediatr Orthopad (2010), 30(1):50-56.
24- Scannell BP, Brighton BK, VanderHave KL. Neurological and Vascular Complications Associated with Supracondylar Humeral Fractures in Children. BJS Rev (2015), 3:1-10.