ABSTRACT
Objective: In this
clinical observational study we assessed the response of atrophic scars of
different etiologies to minor surgical treatment using subcision (subcutaneous
incisional surgery) and platelet-rich plasma injection.
Methods: We recruited
patients with atrophic and depressed scarring that are either laser-naïve or
failed treatment with laser, usually due to resultant post-inflammatory
hyperpigmentation or poor response. Subdermal incision (subcision) was
performed and/or autologous platelet-rich plasma was injected superficially
into the scar. Patients were assessed on a scale of 1 to 10. Some patients were
assessed using the Patient and Observer Scar Assessment Scale.
Results: A grade using percentage of improvement
was suggested to record results. Based on the observer (1 to 10) scale before
and after treatment, a classification of excellent, very good, good, and fair
was utilized to correspond to 75%, 50%, 25% and 10% improvement, respectively.
All of the patients had good clinical
improvement. 15% of the patients had excellent improvement, 67% of them had
very good improvement, and 18% had good improvement.
Conclusion: Subcision and platelet-rich plasma
injection seem to be effective and safe methods of treatment of atrophic scarring
of various etiologies and should be utilized more as a substitute or adjuvant
to fractional CO2 resurfacing in cases of atrophic scarring or
potential laser complications.
Keywords: Atrophic scars, subcision, platelet-rich plasma.
JRMS December 2019;26(3): 72-83 :10.12816/0054821
Introduction
Scars are a major functional and cosmetic concern. Patients with scars represent a good group of a dermatological clinic workload. Scars can be classified into hypertrophic (or elevated, including keloids) and atrophic (or depressed).
Atrophic scars may be traumatic, surgical, due to acne or varicella, stretch marks, among other etiologies. Further classification of acne scars includes icepick, boxcar, and rolled scars.Several modalities have been used for treatment for acne scars, including but not limited to chemical peeling, dermabrasion, laser treatment, and microneedling.
Acne scars may also be treated surgically using procedures such as simple scar excision, scar punch elevation, or punch grafting. Other modalities of treatment include tissue augmentation using fat or fillers.1 Atrophic scars show moderate response, limited efficacy and possible side effects to laser resurfacing and some other treatment modalities.2
In this clinical observational study we evaluated the use of platelet-rich plasma injection combined with subcision, with or without fractional laser treatment for atrophic scars of various etiologies.
Methods
We treated 55
patients with atrophic scars of different etiologies, who presented to King
Hussein Medical Center Dermatology Clinic, in the period from July 2016 to
April 2018. All the patients had atrophic scars. Ages were between 7 and 63
years; with an average of 28.1 years and a median of 28 years. 23 (44%) were
males and 31 (56%) were females. The oldest scar was around 40 years old and
the newest was almost 1 year ago. According to the etiology of the scars, 15
(27%) were acne scars, 25 (45%) were traumatic scars, 7 (13%) were
post-varicella scars (6 post-chickenpox and one case of post-zoster scarring),
and 7 (13%) were surgical scars. Two patients (0.04%) had scars due to
resolving hemangiomas but one of them had had partial surgical treatment with a
resultant scar. 53 patients (96%) had facial scars and only two (4%) had scars
on the thigh. 29 patients (53%) were laser-naive and 26 (47%) had had previous
laser treatments but stopped mostly due to poor response. Some of them also had
post-inflammatory hyperpigmentation as an adverse reaction to laser treatments.
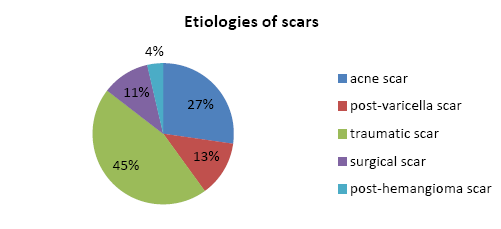
Figure 1: Scar etiologies in our patients
We evaluated
each patient individually. All of the patients had atrophic scars. All of them
were treated using platelet-rich plasma injections and/or subcision.
Platelet-rich plasma was prepared from the patients’ own blood which was drawn
into citrated (sodium citrate, 3.2%) tubes and centrifuged at 2700 rpm for 7
minutes, using our laboratory centrifuge. No commercial kits were used. 8 to 12
ml of blood were drawn to give between 3 and 7 ml of plasma. The amount
differed with each patient (according to the plasma volume) and platelet
concentration was not measured. No specific volume was injected. The lower part
of the supernatant was injected into the superficial dermis until overfilling
was achieved. Sessions were repeated monthly if necessary. Subcision was
performed using a 21-gauge needle, a 25-gauge needle, or an ophthalmic surgical
knife, according to the size and depth of the scar. In most of the patients
lidocaine 2% was injected to the rim of the scar.
Patients were
followed up at least monthly. Results were assessed using a score from 1 to 10
by both the patient and two fixed observers (a specialist dermatologist and a
dermatology nurse, in the same setting) on all patients before and after
treatment; with (1) equivalent to normal skin and (10) equivalent to worst
scar. A similar score was also given by the two observers from our team before
and after treatment. Further assessment by the Patient and Observer Scar
Assessment Scale (POSAS) was implemented on 24 (45%) of the patients.
Results
All of the patients had visible and
measureable clinical improvement. Based on the observer (1 to 10) scale, a
classification of excellent, very good, good, and fair was utilized to
correspond to 75%, 50%, 25% and 10% improvement, respectively. 100% of the
patients had more than 25% (good) improvement in their scars. 8 patients (15%)
had 75% or more (excellent) improvement. 37 patients (67%) had 50% to 75% (very
good) improvement. 10 patients (18%) had 25% to 50% (good) improvement. None of
the patients had less than 25% improvement.
Some of the
patients experienced moderate pain or discomfort during the procedure. A few
patients had transient pigmentary alterations mostly due to extravasated blood,
but none had any longer term side effects.
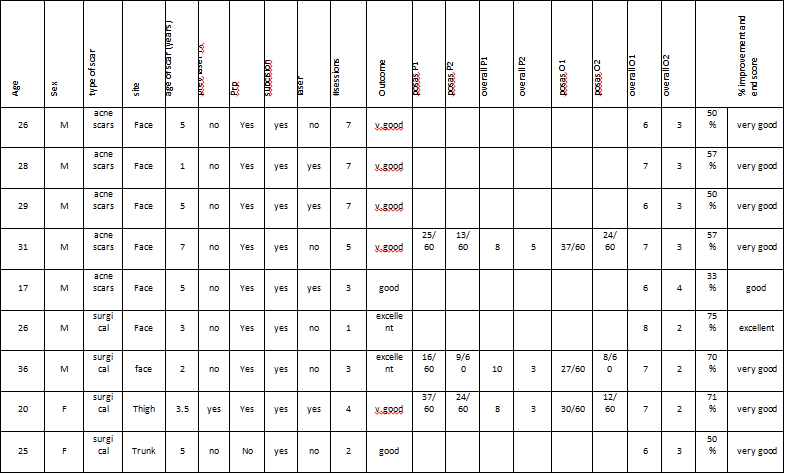
(Table I) shows
how data and results were recorded for each patient.
Table I: sample of the recorded data.
Regarding the
correlation of the age of scars and the percentage of clinical improvement, the
group of patients with scars aged 6-10 years had slightly lower average
improvement than other scar age groups. It is also of note that more chronic
scars showed similar if not higher average improvement to newer ones (Table
II).
Table II:
relation of age of scar to average improvement
|
Age of scar
|
Average improvement
|
|
0-1
|
56%
|
|
2-5
|
57%
|
|
6-10
|
48%
|
|
11+
|
57%
|
As for scar types, we noted that the
best average improvement was achieved in patients with surgical scars (Table
III).
Table III: average improvement by scar type.
|
Average
improvement by Scar Type
|
|
Scar
type
|
average
age of scar
|
sample
size
|
average
age
|
Female
to male percentage
|
Average
number of treatment sessions
|
Average
percentage improvement
|
|
Acne scars
|
8.67
|
15
|
31.73
|
40%
|
3.20
|
47%
|
|
Surgical
|
3.08
|
6
|
25.83
|
67%
|
3.33
|
65%
|
|
Traumatic
|
5.28
|
25
|
28.52
|
56%
|
2.28
|
57%
|
|
Varicella scars
|
5.14
|
7
|
24.57
|
86%
|
2.00
|
50%
|
For the patients who were treated
without subcision (PRP alone), mostly the etiology was traumatic or
post-surgical scars. The average of percentage of improvement was 59% compared
to the average of improvement of patients treated with subcision and PRP or
subcision alone which was 56% (Table IV).
Table IV:
patient characteristics, scar types, and percentage of improvement for patients
not treated with subcision
|
Patient
|
age
|
M/F
|
Subcision (yes/no)
|
scar type
|
#
Sessions
|
%improvement
|
Average %improvement for
scar type
|
|
1
|
21
|
F
|
No
|
surgical
|
7
|
75%
|
67%
|
|
2
|
27
|
F
|
No
|
surgical
|
3
|
50%
|
67%
|
|
3
|
7
|
M
|
No
|
post-hemangioma
|
1
|
75%
|
75%
|
|
4
|
17
|
F
|
No
|
traumatic
|
1
|
40%
|
57%
|
|
5
|
22
|
M
|
No
|
traumatic
|
2
|
78%
|
57%
|
|
6
|
32
|
F
|
No
|
traumatic
|
7
|
50%
|
57%
|
|
7
|
19
|
F
|
No
|
traumatic
|
3
|
60%
|
57%
|
|
8
|
23
|
F
|
No
|
traumatic
|
2
|
57%
|
57%
|
|
9
|
24
|
F
|
No
|
traumatic
|
3
|
40%
|
57%
|
|
10
|
18
|
M
|
No
|
traumatic
|
2
|
57%
|
57%
|
|
11
|
32
|
F
|
No
|
traumatic
|
1
|
63%
|
57%
|
|
Average % improvement without
subcision
|
|
59%
|
|
|
Average % improvement with
subcision
|
|
56%
|
|
Regarding the effect of previous laser
treatment, there was no significant difference between laser-naive and
laser-exposed patients, as shown in (Table V) below.
Table V: The effect of previous laser treatment on
average percentage improvement by scar type
|
The effect of previous laser treatment on average percentage
improvement by scar type
|
|
Scar
type
|
Previous
laser treatment – Yes
|
Previous
laser treatment - No
|
|
acne
scars
|
48%
|
45%
|
|
post
hemangioma
|
-
|
75%
|
|
surgical
|
68%
|
61%
|
|
surgical
and hemangioma
|
-
|
77%
|
|
traumatic
|
63%
|
54%
|
|
varicella
scars
|
56%
|
46%
|
|
Overall
average improvement
|
54%
|
56%
|
Three of the patients were treated with
subcision alone without PRP. (Table VI)
Table VI:
patients treated with subcision without PRP.
|
patient
|
age
|
sex
|
scar type
|
#sessions
|
%improvement
|
%improvement for scar type
|
|
1
|
28
|
M
|
post-acne
|
1
|
50%
|
47%
|
|
2
|
25
|
F
|
varicella
|
1
|
50%
|
50%
|
|
3
|
25
|
F
|
surgical (abdomen)
|
2
|
50%
|
67%
|
|
average
% improvement
|
|
50%
|
|
|
average
% improvement with PRP
|
|
55%
|
|
Figures (1) and (2) show a
post-traumatic scar on the face of a 35-year-old male patient before and after
treatment, respectively.

Figure 1 & 2: before and after treatment. Although the second photograph
is slightly brighter, nevertheless, there is pronounced improvement.
Discussion
Scars can be classified according to color and texture. Scars can be further classified into hypertrophic (elevated) and atrophic (depressed) scars. Atrophic scarring can result from different etiologies including trauma, surgery, post-acne or post-varicella infection. Acne scars are depressed scars and can be further classified into icepick, boxcar, and rolled scars.
Atrophic scars are generally hard to treat compared to hypertrophic scars. Various modalities have been used to treat acne scars with variable results. These include chemical peeling, dermabrasion, laser treatment, and microneedling. Acne scars may also be treated surgically using procedures such as simple scar excision, scar punch elevation, or punch grafting. Other modalities of treatment include tissue augmentation using fat or fillers.3 Many studies have been published regarding treatment of atrophic scars; with the majority of them being observational and most yielding positive results. Nevertheless, there is still paucity of good-quality clinical evidence evaluating treatment modalities for atrophic scars.4
Chemical reconstruction of skin scars using trichloroacetic acid “TCA CROSS” method was originally described by Lee et al for depressed acne scars in patients with Fitzpatrick skin types IV-V. 5 Either 65% or 100% trichloroacetic acid (TCA) was applied to depressed scars for 10 seconds. All patients in the 100% TCA group showed excellent results, and all patients had good satisfaction and no significant complications.
Subcision was suggested in 1995 by Orentreich and Orentreich, who described subcuticular undermining of the scars using a hypodermic tri-beveled needle to lift up and release the scar.6
Triple combination therapy for atrophic acne scar treatment using dot peeling, subcision, and fractional laser was suggested by Kang WH et al and yielded good results. Another combination therapy using subcision, microneedling, and 15% TCA peel was performed on 50 patients with good results in both mild and severe acne scars.7
A split-face comparative study comparing subcision to 100% trichloroacetic acid in the treatment of rolling acne scars in patients with Fitzpatrick skin types III and IV showed better results with subcision and fewer side effects, which were in the form of pigmentary alteration with the TCA CROSS method.8
Another very recent split-face comparative study by V.A. Belgaumkar and N.S. Deshmukh looked at autologous PRP and subcision in comparison with subcision alone in acne scars. It showed greater improvement using the combination treatment.9
In our study, we assessed each patient individually. Some patients had undergone fractional CO2 laser treatments with poor outcome or post-inflammatory hyperpigmentation, in those patients we started with platelet-rich plasma injections with or without subcision.
45 of 55 patients underwent subcision, or subdermal incision. We used a 21-gauge needle, a 25-gauge needle, or an ophthalmic surgical knife, according to the size and depth of the scar. The other 10 patients who did not undergo subcision had post-surgical or post-traumatic atrophic scars with no tethering to underlying dermis. Generally, all patients with acne and varicella scars required subcision.
52 of the 55 patients had platelet-rich plasma injection. The plasma was drawn from patient’s own blood into citrated tubes and then centrifuged at an average of 2700 rpm for 7 minutes. The lower part of the supernatant was injected into the worst part of the scar. The upper part (which represents platelet-poor plasma) was also utilized in the less scarred areas. The treatment was repeated monthly if necessary. The other three patients who did not receive plasma had very good improvement on subcision alone (one post-varicella, one traumatic, and one post-surgical scar).
Most of the patients underwent combination sessions of both subcision and platelet-rich plasma injection. For optimal results, subcision was performed in the first session, and platelet-rich plasma injections were done in subsequent sessions along with minor subcision if needed.
A group of patient did not undergo subcision, because their scars were not adherent to the dermis and had no obvious tethering or fibrosis in order to be modified surgically. That probably explains why the average of percentage of improvement in this subset is not less than the average in the patients treated with combination of platelet-rich plasma and subcision, and shows that platelet-rich plasma as a monotherapy can be effective in selected patients.
The number of sessions performed varied from one to 7, according to clinical response and time limit of the study. 20 patients (36%) underwent one combination session only, 14 patients (25.4%) had 2 sessions, 7 patients (13%) had 3 sessions, 6 (11%) patients had 4 sessions, one patient (1%) had 5 sessions, and 7 (13%) patients underwent 7 sessions with a median of 2 sessions.
Results were obtained on each follow up visit, and recorded on the final visit of the patient. A (1 – 10) observer scale was obtained from all patients. Additional patient and observer scar assessment scale (POSAS) was taken from 22 patients. In addition to clinical assessment, we employed the POSAS in an attempt to find an objective and precise scale which correlates with the patients’ clinical condition.
Many scaling systems have been used in assessment of burn or post surgical scars. The best known are the Vancouver Scar Scale, Seattle Scar Scale, Manchester Scar Scale, and Hamilton Scar Scale, among others. Most do not take into consideration the subjective assessment of the patient, and most do not grade atrophic scarring.10, 11, 12
Goodman and Baron described a grading system for acne scarring that is now widely used, but is specific for post-acne scarring.13
The POSAS was introduced as the first scar scale to have a subjective assessment and includes a patient assessment and an observer assessment. It was developed for all scars and it also takes into account itching and pain. The patient’s parameters include pain, itching, color, stiffness, thickness, and irregularity. Observer assessment includes vascularity, pigmentation, thickness, relief, pliability, and surface area of the scar. The grading for each is added up to a sum of 60. The POSAS also gives an overall assessment of 1-10 by both the patient and the observer.14
A modified POSAS scale was suggested by Fearmonti et al15 and it includes assessment of functional impairment of scars.
Layton et al suggested new patient oriented tools for assessing atrophic acne scarring; the self-assessment for clinical acne-related scars “SCARS” and the facial acne scar quality of life “FASQol”. They assess the psychological impact of acne scars.16
We attempted to use the POSAS on a subset of our patients and to correlate the results with the (1 - 10) before and after scores. 22 patients from our study were assessed using the POSAS. To make the comparison, the resultant score (out of 60) was converted into a score from 10, and was compared to the overall score of 10, for both patient and observer.
The first line graph below (Figure 3) shows the patient-derived scores. A prominent feature is the consistently higher overall score given by patients compared to the score calculated from patient POSAS. This for us indicates that other factors, like psychological, functional, and affected area might influence the overall patient’s opinion that need to be taken into consideration. It is also of note that there is greater improvement using the overall scale, and that also might be related to the un-assessed factors suggested above.
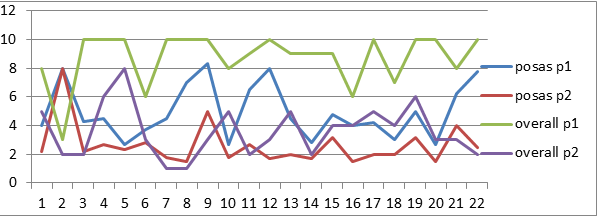
Figure 3: Patient derived scores from POSAS on our subset of 22
patients.
The second line
graph (Figure 4) depicts the observer-derived scores. It is notable that there
is less discrepancy than patient-derived scores, with higher overall scores.
That also can be attributed to other observer unmeasured factors like affected
areas, and to unmeasured patient-derived factors.
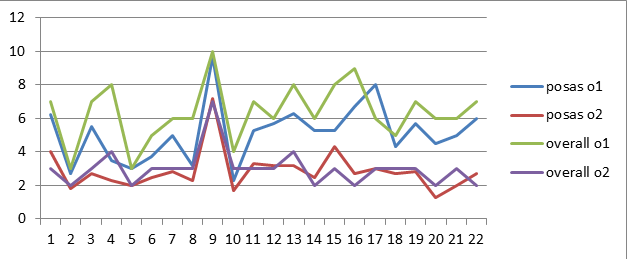
Figure 4: Observer-derived scores from POSAS on our subset of 22
patients.
Conclusion
Scars of all types
especially atrophic are generally difficult to treat and have a psychosocial
and sometimes functional impact on patients.
Platelet-rich
plasma and subcision in combination or alone are effective and safe methods for
the treatment of various scars of different etiologies.
Scar
assessment scales for atrophic scarring need to be more comprehensive. There is
a need to include various scar characteristics due to different etiologies. As
scars, especially post-traumatic, affect patients’ psychological status, more
attention should be given to this issue. Therefore, scar assessment scales need
to be more patient-oriented and to take into consideration the location,
functional, and psychosocial impairment due to scarring.
References
1. Fabbrocini, G. et al. Acne scars:
Pathogenesis, Classification, and Treatment, Dermatol Res Pract 2010 Oct.
2. Gozali MV. Zhou B
Effective Treatments of Atrophic Acne Scars, J Clin Aesthet Dermatol, 2015
May;8(5):33-40
3. Kwok, T and Rao, J. A Practical
Approach to Classification and Treatment of Scars, STL FP Volume 7 Number 6
4. Patel
L, McGrouther D, and Chakrabarty K.
Evaluating Evidence for Atrophic Scarring Treatment Modalities, JRSM Open. 2014
Sep; 5(9)
5. Lee, Kwang Hoon et al. Focal Treatment
of Acne Scars With Trichloroacetic Acid: Chemical Reconstruction of Skin Scars
Method. Dermatol Surg. 2002 Nov:6(11):1017-1021
6. Orentreich DS and Orentreich N. Subcutaneous
Incisionless (Subcision) Surgery for the Correction of Depressed Scars and
Wrinkles. Dermatol Surg. 1995 Jun;21(6):543-9.
7. Kang WH, Kim YJ, Pyo WS, Park SJ,
Kim JH.
Atrophic acne scar treatment using triple combination therapy: dot peeling,
subcision, and fractional laser, J Cosmet Laser Ther. 2009 Dec; 11(4) 212-5.
8. El-Tobshy, Seham Ahmed et al. Subcision
Versus 100% Trichloroacetic Acid in the Treatment of Rolling Acne Scars.
Dermatol Surg. 2011 May;37(5):626-633.
9. Belgaumkar, Vasudha A and
Deshmukh, Nitika S.
Platelet-Rich Plasma Augments Subcision in Atrophic Acne Scars, A Split-Face
Comparative study. Dermatol Surg. 2019 Jan;45(1): 90-98.
10. Fearmonti R. et
al. A Review of Scar Scales and Scar
Measuring Devices. Eplasty. 2010; 10: e43. Published online 2010 Jun 21.
11. Nguyen et al. A
Review of Scar Assessment Scales. Seminars in Cutaneous Medicine and Surgery.
Vol. 34, March 2015.
12. Idriss and Maibach. Review, Scar
Assessment Scales: a Dermatologic Overview. Skin Research and Technology 2009;
15: 1–5
13. Goodman GJ and Baron JA. Postacne Scarring:
A Qualitative Global Scarring Grading System. Dermatol Surg. 2006
Dec;32(12):1458-66.
14. The Patient and Observer Scar
Assessment Scale, Available from: www.posas.org
15. Fearmonti et al. The Modified POSAS: A Novel Approach to Defining Pathologic
and Non-Pathologic Scarring. Plast Reconstr Surg. 2011 Jan: 127(1): 242-247.
16. Layton et al. New Patient-Oriented Tools for Assessing Atrophic Acne
Scarring. Dermatol Ther (Heidelb).
2016 Jun; 6(2): 219–233.
17. Garg
S, Baveja S. Combination therapy in the
management of atrophic acne scars. J Cutan Aesthet Surg 2014;7:18-23
18. Abdel Hay R et al. Interventions
for Acne Scars, Cochrane Database Syst Rev. 2016 Apr3;4
19. Hession MT, Graber EM.
Atrophic Acne Scarring: a Review of Treatment Options. J Aesthet Dermatol. 2015 Jan; 8(1): 50–58.
20. Chawla S. Split Face
Comparative Study of Microneedling with PRP Versus Microneedling with Vitamin C
in Treating Atrophic Post Acne Scars. J Cutan Aesthet Surg. 2014 Oct-Dec; 7(4): 209–212
21. Ibrahim ZA et at. Therapeutic effect of microneedling and autologous
platelet-rich plasma in the treatment of atrophic scars: A randomized study. J Cosmet Dermatol. 2017 Sep;16(3):388-399. doi: 10.1111/jocd.12356.
Epub 2017 May 14.
22. Afthab Jameela
Wahab et al. Efficacy and safety of platelet rich plasma (PRP) as monotherapy.
Indian Journal of Clinical and Experimental Dermatology, July-September
2017;3(3):119-123
23. Barikbin et at. Blunt Blade Subcision: An Evolution in the
Treatment of Atrophic Acne Scars. Dermatologic Surgery: January 2017 - Volume 43 - Issue - p S57–S63
24. Chae JK et al. Values of a Patient and Observer Scar Assessment Scale to
Evaluate the Facial Skin Graft Scar. Ann Dermatol. 2016
Oct;28(5):615-623. Epub 2016 Sep 30.
25. Draaijers et al. The Patient and Observer Scar Assessment
Scale: A Reliable and Feasible Tool for Scar Evaluation. Plastic & Reconstructive Surgery 113(7):1960-1965 · June 2004.
26. Nofal
E. et al. Platelet-rich
Plasma versus CROSS Technique with 100% Trichloroacetic Acid Versus Combined
Skin Needling and Platelet rich Plasma in the Treatment of Atrophic Acne Scars:
A Comparative Study. Dermato Surg. 2014 Aug;40(8):864-73.
27. Keen
A. et al.
Treatment of Post-burn and Post-traumatic Atrophic Scars with Fractional CO2
laser: Experience at a Tertiary Care Center. Lasers Med Sci. 2016 Feb 23.
28. Al-Taweel AI et al. Comparative
Study of the Efficacy of Platelet-rich Plasma Combined with Carboxytherapy vs
Its Use with Fractional Carbon Dioxide Laser in Atrophic Acne Scars. J.Cosmet
Dermatol. 2018 Apr 22.